- Record: found
- Abstract: found
- Article: found
Interventions to Reduce Antibiotic Prescribing in LMICs: A Scoping Review of Evidence from Human and Animal Health Systems

Read this article at
Abstract
This review identifies evidence on supply-side interventions to change the practices of antibiotic prescribers and gatekeepers in low- and middle-income countries (LMICs). A total of 102 studies met the inclusion criteria, of which 70 studies evaluated interventions and 32 provided insight into prescribing contexts. All intervention studies were from human healthcare settings, none were from animal health. Only one context study examined antibiotic use in animal health. The evidence base is uneven, with the strongest evidence on knowledge and stewardship interventions. The review found that multiplex interventions that combine different strategies to influence behaviour tend to have a higher success rate than interventions based on single strategies. Evidence on prescribing contexts highlights interacting influences including health system quality, education, perceptions of patient demand, bureaucratic processes, profit, competition, and cultures of care. Most interventions took place within one health setting. Very few studies targeted interventions across different kinds of providers and settings. Interventions in hospitals were the most commonly evaluated. There is much less evidence on private and informal private providers who play a major role in drug distribution in LMICs. There were no interventions involving drug detailers or the pharmaceutical companies despite their prominent role in the contextual studies.
Related collections
Most cited references85
- Record: found
- Abstract: found
- Article: found
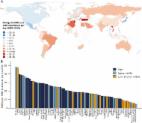
Global increase and geographic convergence in antibiotic consumption between 2000 and 2015
- Record: found
- Abstract: found
- Article: not found