- Record: found
- Abstract: not found
- Article: not found
Ongoing strategies to improve the management of upper respiratory tract infections and reduce inappropriate antibiotic use particularly among lower and middle-income countries: findings and implications for the future
Brian Godman
1
,
2
,
3
,
4 ,
Mainul Haque
5 ,
Judy McKimm
6 ,
Muhamad Abu Bakar
7 ,
Jacqueline Sneddon
8 ,
Janney Wale
9 ,
Stephen Campbell
10
,
11 ,
Antony P. Martin
3 ,
Iris Hoxha
12 ,
Vafa Abilova
13 ,
Bene D. Anand Paramadhas
14 ,
Pinkie Mpinda-Joseph
15 ,
Matshediso Matome
16 ,
Livia Lovato Pires de Lemos
17
,
18 ,
Israel Sefah
19 ,
Amanj Kurdi
1
,
20 ,
Sylvia Opanga
21 ,
Arianit Jakupi
22 ,
Zikria Saleem
4
,
23 ,
Mohamed Azmi Hassali
4 ,
Dan Kibuule
24 ,
Joseph Fadare
25 ,
Tomasz Bochenek
26 ,
Celia Rothe
26 ,
Jurij Furst
27 ,
Vanda Markovic-Pekovic
28 ,
Ljubica Bojanić
29
,
30 ,
Natalie Schellack
2 ,
Johanna C. Meyer
2 ,
Zinhle Matsebula
31 ,
Thuy Nguyen Thi Phuong
32 ,
Binh Nguyen Thanh
32 ,
Saira Jan
33
,
34 ,
Aubrey Kalungia
35 ,
Sekesai Mtapuri-Zinyowera
36 ,
Massimo Sartelli
37 ,
Ruaraidh Hill
38
December 30 2019
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Related collections
Most cited references278
- Record: found
- Abstract: found
- Article: not found
Antibiotic resistance-the need for global solutions.
Ramanan Laxminarayan, Adriano Duse, Chand Wattal … (2013)
- Record: found
- Abstract: found
- Article: found
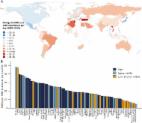
Global increase and geographic convergence in antibiotic consumption between 2000 and 2015
Eili Klein, Thomas P Van Boeckel, Elena M Martinez … (2018)

