- Record: found
- Abstract: found
- Article: not found
COVID‐19, adaptative immune response and metabolic‐associated liver disease
Read this article at
Abstract
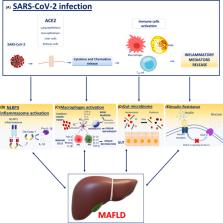
Metabolic diseases are associated with a higher risk of a severer coronavirus disease 2019 (COVID‐19) course, since fatty liver is commonly associated with metabolic disorders, fatty liver itself is considered as a major contributor to low‐grade inflammation in obesity and diabetes. Recently a comprehensive term, metabolic (dysfunction) associated fatty liver disease (MAFLD), has been proposed. The hepatic inflammatory status observed in MAFLD patients is amplified in presence of severe acute respiratory syndrome coronavirus 2 infection. Intestinal dysbiosis is a powerful activator of inflammatory mediator production of liver macrophages. The intestinal microbiome plays a key role in MAFLD progression, which results in non‐alcoholic steatohepatitis and liver fibrosis. Therefore, patients with metabolic disorders and COVID‐19 can have a worse outcome of COVID‐19. This literature review attempts to disentangle the mechanistic link of MAFLD from COVID‐19 complexity and to improve knowledge on its pathophysiology.
Related collections
Most cited references74
- Record: found
- Abstract: found
- Article: not found
Clinical Characteristics of Coronavirus Disease 2019 in China
- Record: found
- Abstract: found
- Article: not found
Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study
- Record: found
- Abstract: found
- Article: not found
