- Record: found
- Abstract: found
- Article: found
Epidemiology of invasive pneumococcal infections: manifestations, incidence and case fatality rate correlated to age, gender and risk factors
Read this article at
Abstract
Background
Incidence, manifestations and case-fatality rate (CFR) of invasive pneumococcal disease (IPD) vary with age and comorbidities. New vaccines, changing age distribution, prolonged survival among immunocompromised patients and improved sepsis management have created a need for an update of basic facts to inform vaccine recommendations.
Methods
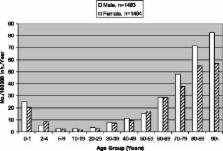
Age, gender and comorbidities were related to manifestations and death for 2977 consecutive patients with IPD in a Swedish region with 1.5 million inhabitants during 13 years before introduction of pneumococcal conjugate vaccines (PCV) in the infant vaccination program. These data were related to population statistics and prevalence of several comorbidities, and compared with two previous studies giving a total follow-up of 45 years in the same area.
Results
The annual incidence was 15/100,000 for any IPD and 1.1/100,000 for meningitis; highest among elderly followed by children < 2 years. It was 2238/100,000 among myeloma patients, followed by chronic lymphatic leukemia, hemodialysis and lung cancer, but not elevated among asthma patients. CFR was 10 % among all patients, varying from 3 % below 18 years to 22 % ≥ 80 years. During 45 years, the IPD incidence increased threefold and CFR dropped from 20 to 10 %. Meningitis incidence remained stable (1.1/100,000/year) but CFR dropped from 33 to 13 %. IPD-specific mortality decreased among children <2 years from 3.1 to 0.46/100,000/year but tripled among those ≥65 years.
Related collections
Most cited references33
- Record: found
- Abstract: found
- Article: not found
Invasive pneumococcal disease caused by nonvaccine serotypes among alaska native children with high levels of 7-valent pneumococcal conjugate vaccine coverage.
- Record: found
- Abstract: found
- Article: not found
Updated recommendations for prevention of invasive pneumococcal disease among adults using the 23-valent pneumococcal polysaccharide vaccine (PPSV23).
- Record: found
- Abstract: found
- Article: not found