- Record: found
- Abstract: found
- Article: found
Computational models of atrial fibrillation: achievements, challenges, and perspectives for improving clinical care

Read this article at
Abstract
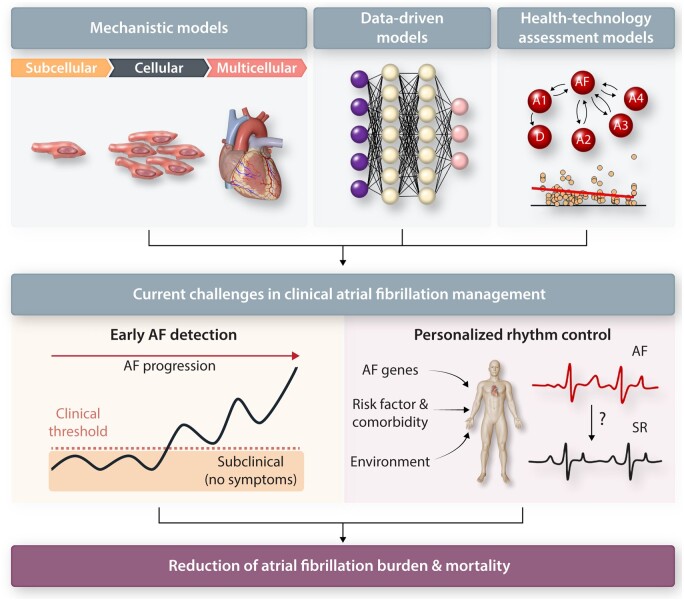
Despite significant advances in its detection, understanding and management, atrial fibrillation (AF) remains a highly prevalent cardiac arrhythmia with a major impact on morbidity and mortality of millions of patients. AF results from complex, dynamic interactions between risk factors and comorbidities that induce diverse atrial remodelling processes. Atrial remodelling increases AF vulnerability and persistence, while promoting disease progression. The variability in presentation and wide range of mechanisms involved in initiation, maintenance and progression of AF, as well as its associated adverse outcomes, make the early identification of causal factors modifiable with therapeutic interventions challenging, likely contributing to suboptimal efficacy of current AF management. Computational modelling facilitates the multilevel integration of multiple datasets and offers new opportunities for mechanistic understanding, risk prediction and personalized therapy. Mathematical simulations of cardiac electrophysiology have been around for 60 years and are being increasingly used to improve our understanding of AF mechanisms and guide AF therapy. This narrative review focuses on the emerging and future applications of computational modelling in AF management. We summarize clinical challenges that may benefit from computational modelling, provide an overview of the different in silico approaches that are available together with their notable achievements, and discuss the major limitations that hinder the routine clinical application of these approaches. Finally, future perspectives are addressed. With the rapid progress in electronic technologies including computing, clinical applications of computational modelling are advancing rapidly. We expect that their application will progressively increase in prominence, especially if their added value can be demonstrated in clinical trials.
Graphical Abstract
Related collections
Most cited references165
- Record: found
- Abstract: found
- Article: not found