- Record: found
- Abstract: found
- Article: found
Causes and predictors of mortality in biopsy-proven lupus nephritis: the Sarawak experience
Read this article at
Abstract
Background
Lupus nephritis (LN) is a serious manifestation of systemic lupus erythematosus that can be fatal if left untreated. The causes and prognostic predictors of mortality in LN have been well studied in developed countries but evidence is lacking for developing countries. The objective of this study was to investigate the causes and predictors of mortality in a cohort of Malaysian patients with biopsy-proven LN.
Methods
We retrospectively studied all patients with biopsy-proven LN treated in Sarawak General Hospital during the period of 2000–15. Demographic data, clinical features and outcomes were collected. Cox regression analysis was carried out to determine the independent predictors of mortality.
Results
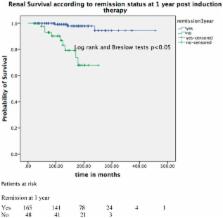
There was a total of 250 patients with 259 renal biopsies available for our analysis. Our patients were of multi-ethnic origins with a female predominance (90%). Their mean ± standard deviation age was 37.7 ± 12.8 years. The patients had a mean disease duration of 135.6 ± 81.9 months. Nephrotic syndrome was the most common presentation (29.6%) and acute renal failure was evident at initial presentation in 16% of patients. Class IV LN was the predominant biopsy class within the cohort (66.8%). The majority of patients achieved remission (81.2%) and had normal renal function (83.9%) at the last follow-up. The 5-, 10-, 15- and 20-year survival rates for our cohort were 93%, 88%, 82% and 77%, respectively. There were 37 deaths (14.8%), of which the main causes were: infection and flare (52.7%), infection alone (25.0%) and other causes (22.3%). Independent predictors of mortality in our cohort of LN patients were: the presence of acute kidney injury at presentation [hazard ratio (HR) 3.41; confidence interval (CI) 1.50–7.76], failure to achieve remission at 1-year post-induction therapy (HR 2.99; CI 1.35–6.65) and non-compliance with treatment (HR 1.89; CI 1.22–2.96). Age, ethnicity, class of LN and type of immunosuppressant used were not predictive of mortality.
Conclusions
Survival and renal outcomes in our LN cohort were comparable to most LN studies reported worldwide. Both flare and infection remained the main causes of death. The presence of acute renal failure at presentation, failure to achieve remission at 1 year post-treatment and non-compliance with treatment were independent prognostic predictors of mortality in LN.
Related collections
Most cited references16
- Record: found
- Abstract: found
- Article: not found
Clinical efficacy and side effects of antimalarials in systemic lupus erythematosus: a systematic review.
- Record: found
- Abstract: found
- Article: found
The frequency and outcome of lupus nephritis: results from an international inception cohort study.
- Record: found
- Abstract: found
- Article: not found