- Record: found
- Abstract: found
- Article: not found
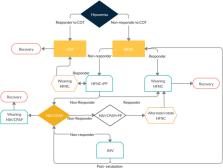
Non-invasive respiratory support paths in hospitalized patients with COVID-19 proposal of an algorithm
Read this article at
Abstract
COVID-19 related Acute Respiratory Failure, may be successfully treated with Conventional Oxygen therapy, High Flow Nasal Cannula, Continuous Positive Airway Pressure or Bi-level Positive-Pressure ventilation. Despite the accumulated data in favor of the use of different Non-invasive Respiratory therapies in COVID-19 related Acute Respiratory Failure, it is not fully understood when start, escalate and de-escalate the best respiratory supportive option for the different timing of the disease. Based on the current published experience with Non-invasive Respiratory therapies in COVID-19 related Acute Respiratory Failure, we propose an algorithm in deciding when to start, when to stop and when to wean different NIRT. This strategy may help clinicians in better choosing NIRT during this second COVID-19 wave and beyond.
Related collections
Most cited references66
- Record: found
- Abstract: found
- Article: not found
Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19)
- Record: found
- Abstract: found
- Article: not found
Pathophysiology of COVID-19-associated acute respiratory distress syndrome: a multicentre prospective observational study
- Record: found
- Abstract: found
- Article: not found
