- Record: found
- Abstract: found
- Article: found
A survey of the current use of neuromuscular blocking drugs among the Middle Eastern anesthesiologists
Read this article at
Abstract
Background:
This survey aimed to assess the extent of practice of the Middle Eastern anesthesiologists in the use of neuromuscular blocking agents (NMB) in 2012.
Methods:
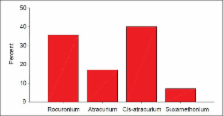
We distributed an electronic survey among 577 members of the Triple-M Middle Eastern Yahoo anesthesia group, enquiring about their practice in the use of neuromuscular blocking agents. Questions concerned the routine first choice use of NMB, choice for tracheal intubation, the use of neuromuscular monitoring (NMT), type of NMB used in difficult airway, frequency of using suxamethonium, cisatracurium, rocuronium and sugammadex, observed side effects of rocuronium, residual curarization, and the reversal of residual curarization of rocuronium.
Results:
A total of 71 responses from 22 Middle Eastern institutions were collected. Most of the Middle Eastern anesthesiologists were using cisatracurium and rocuronium frequently for tracheal intubation (39% and 35%, respectively). From the respondents, 2/3 were using suxamethonium for tracheal intubation in difficult airway, 1/3 were using rocuronium routinely and 17% have observed hypersensitivity reactions to rocuronium, 54% reported residual curarization from rocuronium, 78% were routinely using neostigmine to reverse the rocuronium, 21% used sugammadex occasionally, and 35% were using NMT routinely during the use of NMB.
Conclusions:
We believe that more could be done to increase the awareness of the Middle Eastern anesthesiologists about the high incidence of PROC (>20%) and the need for routine monitoring of neuromuscular function. This could be accomplished with by developing formal training programs and providing official guidelines.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
A survey of current management of neuromuscular block in the United States and Europe.
- Record: found
- Abstract: found
- Article: not found
Rapid sequence induction and intubation with rocuronium-sugammadex compared with succinylcholine: a randomized trial.
- Record: found
- Abstract: found
- Article: not found