- Record: found
- Abstract: found
- Article: found
Primary central nervous system tumors survival in children in ten Colombian cities: a VIGICANCER report
Read this article at
Abstract
Purpose
Primary central nervous system (CNS) tumors are the second most common cancer in children and adolescents, leading to premature death and disability. Population-based survival estimates aid decision-making in cancer control, however data on survival for primary CNS tumors in Latin America is lacking. We describe survival rates for children with primary CNS tumors treated in ten Colombian cities.
Methods
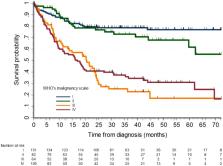
We analyzed data from children and adolescents newly diagnosed with cancer between 2012 and 2021, participating in the Childhood Cancer Clinical Outcomes Surveillance System (VIGICANCER) in ten cities in Colombia. VIGICANCER collects information on clinical outcomes from twenty-seven pediatric oncology units and conducts active follow-up every three months. VIGICANCER does not register craniopharyngiomas; we excluded intracranial germ cell tumors for this report. We used the Kaplan-Meier method to estimate the overall survival probability, stratified by sociodemographic variables, topography, WHO grading, receipt of radiation therapy, and type of surgical resection. We analyzed the prognostic capacity of variables using multivariate proportional Cox’s regression, stratified by city and year of diagnosis.
Results
During the study period, VIGICANCER included 989 primary CNS tumors in 879 children and 110 adolescents. The cohort median age was 9 years; 53% of patients were males, and 8% were Afro-descendants. Most common tumors were supratentorial astrocytomas (47%), astrocytic tumors (35%), medulloblastomas (20%), ependymomas (11%), and mixed and unspecified gliomas (10%). Five-year overall survival of the entire cohort was 54% (95% CI, 51-58); for supratentorial gliomas, WHO grade I was 77%, II was 62%, III-IV was 27%, respectively, and for medulloblastoma was 61%. The adjusted hazard rate ratio for patients with WHO grade III and IV, for those with subtotal resection, for brainstem location, and for those not receiving radiation therapy was 7.4 (95% CI, 4.7–11.8), 6.4 (95% CI, 4.2–9.8), 2.8 (95% 2.1–3.8), 2.0 (95% CI, 1.3–2.8) and 2.3 (95% CI, 1.7–3.0), respectively.
Conclusion
We found that half of Colombia’s children and adolescents with primary CNS tumors survive five years, compared to 70% to 80% in high-income countries. In addition to tumor biology and location, gross total resection was crucial for improved survival in this cohort. Systematic monitoring of survival and its determinants provides empirical data for guiding cancer control policies.
Related collections
Most cited references36
- Record: found
- Abstract: found
- Article: not found
The 2007 WHO Classification of Tumours of the Central Nervous System

- Record: found
- Abstract: found
- Article: found