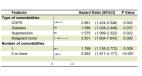
China and the rest of the world are experiencing an outbreak of a novel betacoronavirus known as severe acute respiratory syndrome corona virus 2 (SARS-CoV-2). 1 By Feb 12, 2020, the rapid spread of the virus had caused 42 747 cases and 1017 deaths in China and cases have been reported in 25 countries, including the USA, Japan, and Spain. WHO has declared 2019 novel coronavirus disease (COVID-19), caused by SARS-CoV-2, a public health emergency of international concern. In contrast to severe acute respiratory system coronavirus and Middle East respiratory syndrome coronavirus, more deaths from COVID-19 have been caused by multiple organ dysfunction syndrome rather than respiratory failure, 2 which might be attributable to the widespread distribution of angiotensin converting enzyme 2—the functional receptor for SARS-CoV-2—in multiple organs.3, 4 Patients with cancer are more susceptible to infection than individuals without cancer because of their systemic immunosuppressive state caused by the malignancy and anticancer treatments, such as chemotherapy or surgery.5, 6, 7, 8 Therefore, these patients might be at increased risk of COVID-19 and have a poorer prognosis. On behalf of the National Clinical Research Center for Respiratory Disease, we worked together with the National Health Commission of the People's Republic of China to establish a prospective cohort to monitor COVID-19 cases throughout China. As of the data cutoff on Jan 31, 2020, we have collected and analysed 2007 cases from 575 hospitals (appendix pp 4–9 for a full list) in 31 provincial administrative regions. All cases were diagnosed with laboratory-confirmed COVID-19 acute respiratory disease and were admitted to hospital. We excluded 417 cases because of insufficient records of previous disease history. 18 (1%; 95% CI 0·61–1·65) of 1590 COVID-19 cases had a history of cancer, which seems to be higher than the incidence of cancer in the overall Chinese population (285·83 [0·29%] per 100 000 people, according to 2015 cancer epidemiology statistics 9 ). Detailed information about the 18 patients with cancer with COVID-19 is summarised in the appendix (p 1). Lung cancer was the most frequent type (five [28%] of 18 patients). Four (25%) of 16 patients (two of the 18 patients had unknown treatment status) with cancer with COVID-19 had received chemotherapy or surgery within the past month, and the other 12 (25%) patients were cancer survivors in routine follow-up after primary resection. Compared with patients without cancer, patients with cancer were older (mean age 63·1 years [SD 12·1] vs 48·7 years [16·2]), more likely to have a history of smoking (four [22%] of 18 patients vs 107 [7%] of 1572 patients), had more polypnea (eight [47%] of 17 patients vs 323 [23%] of 1377 patients; some data were missing on polypnea), and more severe baseline CT manifestation (17 [94%] of 18 patients vs 1113 [71%] of 1572 patients), but had no significant differences in sex, other baseline symptoms, other comorbidities, or baseline severity of x-ray (appendix p 2). Most importantly, patients with cancer were observed to have a higher risk of severe events (a composite endpoint defined as the percentage of patients being admitted to the intensive care unit requiring invasive ventilation, or death) compared with patients without cancer (seven [39%] of 18 patients vs 124 [8%] of 1572 patients; Fisher's exact p=0·0003). We observed similar results when the severe events were defined both by the above objective events and physician evaluation (nine [50%] of 18 patients vs 245 [16%] of 1572 patients; Fisher's exact p=0·0008). Moreover, patients who underwent chemotherapy or surgery in the past month had a numerically higher risk (three [75%] of four patients) of clinically severe events than did those not receiving chemotherapy or surgery (six [43%] of 14 patients; figure ). These odds were further confirmed by logistic regression (odds ratio [OR] 5·34, 95% CI 1·80–16·18; p=0·0026) after adjusting for other risk factors, including age, smoking history, and other comorbidities. Cancer history represented the highest risk for severe events (appendix p 3). Among patients with cancer, older age was the only risk factor for severe events (OR 1·43, 95% CI 0·97–2·12; p=0·072). Patients with lung cancer did not have a higher probability of severe events compared with patients with other cancer types (one [20%] of five patients with lung cancer vs eight [62%] of 13 patients with other types of cancer; p=0·294). Additionally, we used a Cox regression model to evaluate the time-dependent hazards of developing severe events, and found that patients with cancer deteriorated more rapidly than those without cancer (median time to severe events 13 days [IQR 6–15] vs 43 days [20–not reached]; p<0·0001; hazard ratio 3·56, 95% CI 1·65–7·69, after adjusting for age; figure). Figure Severe events in patients without cancer, cancer survivors, and patients with cancer (A) and risks of developing severe events for patients with cancer and patients without cancer (B) ICU=intensive care unit. In this study, we analysed the risk for severe COVID-19 in patients with cancer for the first time, to our knowledge; only by nationwide analysis can we follow up patients with rare but important comorbidities, such as cancer. We found that patients with cancer might have a higher risk of COVID-19 than individuals without cancer. Additionally, we showed that patients with cancer had poorer outcomes from COVID-19, providing a timely reminder to physicians that more intensive attention should be paid to patients with cancer, in case of rapid deterioration. Therefore, we propose three major strategies for patients with cancer in this COVID-19 crisis, and in future attacks of severe infectious diseases. First, an intentional postponing of adjuvant chemotherapy or elective surgery for stable cancer should be considered in endemic areas. Second, stronger personal protection provisions should be made for patients with cancer or cancer survivors. Third, more intensive surveillance or treatment should be considered when patients with cancer are infected with SARS-CoV-2, especially in older patients or those with other comorbidities.