- Record: found
- Abstract: found
- Article: found
Population-based blood screening for preclinical Alzheimer’s disease in a British birth cohort at age 70

Read this article at
Abstract
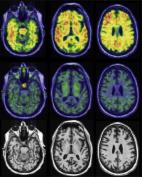
Alzheimer’s disease has a preclinical stage when cerebral amyloid-β deposition occurs before symptoms emerge, and when amyloid-β-targeted therapies may have maximum benefits. Existing amyloid-β status measurement techniques, including amyloid PET and CSF testing, are difficult to deploy at scale, so blood biomarkers are increasingly considered for screening. We compared three different blood-based techniques—liquid chromatography-mass spectrometry measures of plasma amyloid-β, and single molecule array (Simoa) measures of plasma amyloid-β and phospho-tau181—to detect cortical 18F-florbetapir amyloid PET positivity (defined as a standardized uptake value ratio of >0.61 between a predefined cortical region of interest and eroded subcortical white matter) in dementia-free members of Insight 46, a substudy of the population-based British 1946 birth cohort. We used logistic regression models with blood biomarkers as predictors of amyloid PET status, with or without age, sex and APOE ε4 carrier status as covariates. We generated receiver operating characteristics curves and quantified areas under the curves to compare the concordance of the different blood tests with amyloid PET. We determined blood test cut-off points using Youden’s index, then estimated numbers needed to screen to obtain 100 amyloid PET-positive individuals. Of the 502 individuals assessed, 441 dementia-free individuals with complete data were included; 82 (18.6%) were amyloid PET-positive. The area under the curve for amyloid PET status using a base model comprising age, sex and APOE ε4 carrier status was 0.695 (95% confidence interval: 0.628–0.762). The two best-performing Simoa plasma biomarkers were amyloid-β 42/40 (0.620; 0.548–0.691) and phospho-tau181 (0.707; 0.646–0.768), but neither outperformed the base model. Mass spectrometry plasma measures performed significantly better than any other measure (amyloid-β 1-42/1-40: 0.817; 0.770–0.864 and amyloid-β composite: 0.820; 0.775–0.866). At a cut-off point of 0.095, mass spectrometry measures of amyloid-β 1-42/1-40 detected amyloid PET positivity with 86.6% sensitivity and 71.9% specificity. Without screening, to obtain 100 PET-positive individuals from a population with similar amyloid PET positivity prevalence to Insight 46, 543 PET scans would need to be performed. Screening using age, sex and APOE ε4 status would require 940 individuals, of whom 266 would proceed to scan. Using mass spectrometry amyloid-β 1-42/1-40 alone would reduce these numbers to 623 individuals and 243 individuals, respectively. Across a theoretical range of amyloid PET positivity prevalence of 10–50%, mass spectrometry measures of amyloid-β 1-42/1-40 would consistently reduce the numbers proceeding to scans, with greater cost savings demonstrated at lower prevalence.
Abstract
Keshavan et al. show that plasma Aβ 1-42/1-40 and a plasma Aβ composite measured by liquid chromatography–mass spectrometry perform better than various blood biomarkers measured by single molecular array, and better than age, sex and APOE ε4, in screening for preclinical Alzheimer’s disease in the British 1946 birth cohort.
Related collections
Most cited references47
- Record: found
- Abstract: not found
- Article: not found
"Mini-mental state". A practical method for grading the cognitive state of patients for the clinician.
- Record: found
- Abstract: found
- Article: found
NIA-AA Research Framework: Toward a biological definition of Alzheimer’s disease
- Record: found
- Abstract: found
- Article: found