- Record: found
- Abstract: found
- Article: found
Association Between Early Invasive Mechanical Ventilation and Day-60 Mortality in Acute Hypoxemic Respiratory Failure Related to Coronavirus Disease-2019 Pneumonia
Read this article at
Abstract
Supplemental Digital Content is available in the text.
Abstract
Objectives:
About 5% of patients with coronavirus disease-2019 are admitted to the ICU for acute hypoxemic respiratory failure. Opinions differ on whether invasive mechanical ventilation should be used as first-line therapy over noninvasive oxygen support. The aim of the study was to assess the effect of early invasive mechanical ventilation in coronavirus disease-2019 with acute hypoxemic respiratory failure on day-60 mortality.
Patients:
Coronavirus disease-2019 patients with acute hypoxemic respiratory failure (Pa o 2/F io 2 ≤ 300 mm Hg), without shock or neurologic failure on ICU admission, and not referred from another ICU or intermediate care unit were included.
Intervention:
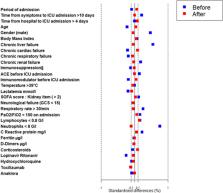
We compared day-60 mortality in patients who were on invasive mechanical ventilation within the first 2 calendar days of the ICU stay (early invasive mechanical ventilation group) and those who were not (nonearly invasive mechanical ventilation group). We used a Cox proportional-hazard model weighted by inverse probability of early invasive mechanical ventilation to determine the risk of death at day 60.
Measurement and Main Results:
The 245 patients included had a median (interquartile range) age of 61 years (52–69 yr), a Simplified Acute Physiology Score II score of 34 mm Hg (26–44 mm Hg), and a Pa o 2/F io 2 of 121 mm Hg (90–174 mm Hg). The rates of ICU-acquired pneumonia, bacteremia, and the ICU length of stay were significantly higher in the early ( n = 117 [48%]) than in the nonearly invasive mechanical ventilation group ( n = 128 [52%]), p < 0.01. Day-60 mortality was 42.7% and 21.9% in the early and nonearly invasive mechanical ventilation groups, respectively. The weighted model showed that early invasive mechanical ventilation increased the risk for day-60 mortality (weighted hazard ratio =1.74; 95% CI, 1.07–2.83, p=0.03).
Related collections
Most cited references47
- Record: found
- Abstract: found
- Article: not found
Acute respiratory distress syndrome: the Berlin Definition.
- Record: found
- Abstract: found
- Article: not found