- Record: found
- Abstract: found
- Article: found
Increasing Incidence of Human Melioidosis in Northeast Thailand
Read this article at
Abstract
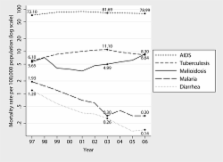
Melioidosis is a serious community-acquired infectious disease caused by the Gram-negative environmental bacterium Burkholderia pseudomallei. A prospective cohort study identified 2,243 patients admitted to Sappasithiprasong Hospital in northeast Thailand with culture-confirmed melioidosis between 1997 and 2006. These data were used to calculate an average incidence rate for the province of 12.7 cases of melioidosis per 100,000 people per year. Incidence increased incrementally from 8.0 (95% confidence interval [CI] = 7.2–10.0) in 2000 to 21.3 (95% CI = 19.2–23.6) in 2006 ( P < 0.001; χ 2 test for trend). Male sex, age ≥ 45 years, and either known or undiagnosed diabetes were independent risk factors for melioidosis. The average mortality rate from melioidosis over the study period was 42.6%. The minimum estimated population mortality rate from melioidosis in 2006 was 8.63 per 100,000 people (95% CI = 7.33–10.11), the third most common cause of death from infectious diseases in northeast Thailand after human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS) and tuberculosis.
Related collections
Most cited references17
- Record: found
- Abstract: found
- Article: not found
The global distribution of Burkholderia pseudomallei and melioidosis: an update.
- Record: found
- Abstract: found
- Article: not found