- Record: found
- Abstract: found
- Article: found
Increased Odds of Death for Patients with Interstitial Lung Disease and COVID-19: A Case–Control Study
letter
Anthony J. Esposito
1 ,
Aravind A. Menon
1 ,
Auyon J. Ghosh
1 ,
Rachel K. Putman
1 ,
Laura E. Fredenburgh
1 ,
Souheil Y. El-Chemaly
1 ,
Hilary J. Goldberg
1 ,
Rebecca M. Baron
1 ,
Gary M. Hunninghake
1 ,
Tracy J. Doyle
1
,
‡
15 December 2020
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
To the Editor:
Coronavirus disease (COVID-19) is an international public health emergency. Although
the prevalence of chronic respiratory disease in patients with COVID-19 has been reportedly
low (1.5%), it is associated with increased risk of severe disease and—in chronic
obstructive pulmonary disease—increased mortality (1–3). Together with numerous previously
reported risk factors for severe COVID-19 (1–6), it has been hypothesized that patients
with interstitial lung diseases (ILDs) may have poorer outcomes from COVID-19 (7).
In this letter, we present the results of a multicenter retrospective case–control
study examining outcomes from COVID-19 in patients with preexisting ILD.
Methods
Adult patients (greater than 18 yr old) with preexisting ILD who had COVID-19 diagnosed
by real-time PCR or with negative real-time PCR but positive IgM and/or IgG serology
between March 1 and June 8, 2020, at six Mass General Brigham hospitals were identified
using the electronic health record–integrated centralized clinical data registry.
ILD was defined as physician diagnosis or, if no pulmonology visit existed in our
system, as radiologic evidence with confirmatory histopathology. Patients with lung
transplantation were excluded. A control cohort with COVID-19 but without ILD was
identified from the same registry and preliminarily matched by age ± 5 years, sex,
white/nonwhite race, and comparative health using an automated method. Control subjects
were confirmed not to have ILD through medical record review, and 2:1 matching was
manually verified. Other than ILD, no other comorbidities were restricted from the
control cohort. Data on demographics, medical history, medications, and outcomes were
collected on both cohorts; pulmonary function, computed tomographic ILD pattern, and
laboratory and therapeutic data were collected on the ILD cohort. The definition of
the usual interstitial pneumonitis (UIP) pattern was inclusive of both definite and
probable radiographic criteria. The primary outcome of interest was death, censored
on June 8, 2020. Secondary outcomes included hospital admission, ICU admission, and
hospital discharge either to the home or a skilled nursing facility. Statistical analyses
were performed with Wilcoxon rank-sum test, Fisher exact test, and simple and multiple
logistic regression adjusting for variables of statistical and clinical interest using
R 3.6.1 (https://www.r-project.org). The study was deemed exempt from informed consent
by the Mass General Brigham Institutional Review Board (protocol 2020P001397).
Results
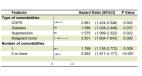
We identified 306 patients with ILD who underwent testing for COVID-19, of whom 46
(15%) were positive and included in our study. Of 3,091 COVID-19–positive patients
without ILD, we selected 92 (3%) control subjects matched for age, sex, and race.
Of note, only one case had negative real-time PCR with positive serologies for both
IgM and IgG. All control subjects had positive real-time PCR results. Fifteen (33%)
of the 46 COVID-19–positive patients with ILD died compared with 12 (13%) of the 92
control subjects without ILD, representing an increased odds ratio of death in patients
with ILD of 3.2 (95% confidence interval, 1.3–7.3; P = 0.01) (Table 1). Increased
mortality was observed even after adjustment for age, sex, race, smoking status, cardiovascular
disease (congestive heart failure and/or coronary artery disease), and any chronic
immunosuppression (odds ratio, 4.3; 95% confidence interval, 1.4–14.0; P = 0.01).
Additional analyses including chronic oxygen supplementation, chronic corticosteroid
use alone, or other chronic immunosuppression did not affect the significance of the
association between ILD and odds of death. Of note, two cases remained hospitalized
at the time of censorship, one of whom was on mechanical ventilation. Compared with
patients without ILD, COVID-19–positive patients with ILD were more likely to be admitted
to the hospital and to require ICU care. Furthermore, they were less likely to be
discharged from the hospital, particularly to the home.
Table 1.
Clinical Characteristics of Patients with COVID-19 and Comorbid ILD Compared with
a Matched Cohort of Patients with COVID-19 without Comorbid ILD
ILD (n = 46)
No ILD (n = 92)
Odds Ratio (95% CI)
P Value
Patient characteristics
Age, yr, median (IQR)
69 (58–78)
69 (59–78)
NA
NS
Sex, M, n (%)
16 (35)
32 (35)
NA
NS
Race, n (%)
NS
White
19 (41)
38 (41)
NA
Black
9 (20)
27 (29)
NA
Hispanic
12 (26)
13 (14)
NA
Other
6 (13)
14 (15)
NA
BMI, kg/m2, median (IQR)
27.6 (22.5–33.2)
28.7 (23.7–33.5)
NA
NS
Smoking status, n (%)
0.07
Never-smoker
19 (41)
57 (62)
NA
Current smoker
4 (9)
5 (5)
NA
Former smoker
23 (50)
30 (33)
NA
Pack-years, median (IQR)
32.5 (15.0–40.0)
15.0 (8.0–27.8)
NA
NS
Comorbidities, n (%)
Diabetes mellitus
16 (35)
31 (34)
NA
NS
Hypertension
35 (76)
62 (67)
NA
NS
Cardiovascular disease
23 (50)
30 (33)
NA
0.06
Obstructive lung disease
15 (33)
25 (27)
NA
NS
Chronic therapies, n (%)
Home oxygen supplementation
5 (11)
3 (3)
NA
NS
Inhaled corticosteroid
10 (22)
15 (16)
NA
NS
Long-acting β-agonist
7 (15)
6 (7)
NA
NS
Long-acting muscarinic antagonist
3 (7)
1 (1)
NA
NS
Corticosteroid
11 (24)
4 (4)
NA
0.001
Other immunosuppression*
18 (39)
7 (8)
NA
<0.001
ACEi/ARB
17 (37)
32 (35)
NA
NS
Nonsteroidal antiinflammatory
7 (15)
8 (9)
NA
NS
Outcomes, n (%)
Hospital admission
†
34 (74)
53 (58)
2.1 (0.9–4.6)
0.07
ICU level of care
16 (47)
12 (23)
3.0 (1.2–7.9)
0.02
Mechanical ventilation
13 (81)
11 (92)
0.4 (0.03–3.1)
NS
Length of stay, d
7 (5–13)
7 (5–14)
NA
NS
Discharged
17 (50)
45 (85)
0.2 (0.06–0.5)
<0.001
Home
9 (28)
31 (58)
0.3 (0.1–0.7)
0.008
Skilled nursing facility
8 (25)
14 (26)
0.9 (0.3–2.6)
NS
Death
15 (33)
12 (13)
3.2 (1.3–7.3)
0.01
Definition of abbreviations: ACEi = angiotensin-converting enzyme inhibitor; ARB = angiotensin
II receptor blocker; BMI = body mass index; CI = confidence interval; COVID-19 = coronavirus
disease; ILD = interstitial lung disease; IQR = interquartile range; NA = not applicable;
NS = not significant (P > 0.1).
*
Other immunosuppression in the ILD cohort includes mycophenolate mofetil (n = 4; 22%),
rituximab (n = 7; 39%), tacrolimus (n = 1; 6%), and other (n = 9; 50%). All seven
non-ILD cohort immunosuppression medications were other (n = 7; 8%).
†
The percentages in subgroups were calculated using the parent group (i.e., the denominator
for ICU level of care was hospital admission).
Comparing survivors and nonsurvivors in the ILD cohort, nonsurvivors were significantly
older (Table 2). We did not find evidence of an association between death from COVID-19
and male sex, race, obesity, smoking status, hypertension, diabetes, cardiovascular
disease, or obstructive lung disease. The UIP pattern, present in 11 (24%) of all
patients with ILD, was more common in nonsurvivors (40% vs. 16%; P = 0.14), although
this was not significantly associated with death in this small subset of cases. Of
those with UIP, antifibrotics were exclusively used by survivors. Overall, investigational
therapies were not associated with death, although there was a trend toward more frequent
treatment with hydroxychloroquine in nonsurvivors.
Table 2.
Clinical Characteristics of Patients with ILD and COVID-19 Stratified by Death
Survivors (n = 31; 67%)
Nonsurvivors (n = 15; 33%)
P Value
Patient characteristics
Age, yr, median (IQR)
67 (55–72)
76 (65–90)
0.02
Sex, M, n (%)
11 (35)
5 (33)
NS
Race/ethnicity, n (%)
NS
White
11 (35)
8 (53)
Black
6 (19)
3 (20)
Hispanic
9 (29)
3 (20)
Other
5 (16)
1 (7)
BMI, kg/m2, median (IQR)
27.9 (22.5–34.0)
24.0 (22.4–31.9)
NS
Smoking status, n (%)
NS
Never-smoker
12 (39)
7 (47)
Former smoker
16 (52)
7 (47)
Current smoker
3 (10)
1 (7)
Pack-years, median (IQR)
35.0 (15.0–47.5)
32.5 (15.3–40.0)
NS
Comorbidities, n (%)
Diabetes mellitus
11 (35)
5 (33)
NS
Hypertension
22 (71)
13 (87)
NS
Cardiovascular disease
15 (48)
8 (53)
NS
Obstructive lung disease
11 (35)
4 (27)
NS
Chronic therapies, n (%)
Home oxygen supplementation
2 (10)
3 (20)
NS
Inhaled corticosteroid
9 (29)
1 (7)
NS
Long-acting β-agonist
6 (19)
1 (7)
NS
Long-acting muscarinic antagonist
1 (3)
2 (13)
NS
Corticosteroid
6 (19)
5 (33)
NS
Other immunosuppression*
11 (35)
7 (47)
NS
Antifibrotic
3 (10)
0 (0)
NS
ACEi/ARB
12 (39)
5 (33)
NS
Nonsteroidal antiinflammatory
4 (13)
3 (20)
NS
Pulmonary characteristics
UIP (definite or probable),
†
n (%)
5 (16)
6 (40)
NS
FEV1% predicted, median (IQR)
81 (67–90)
80 (63–104)
NS
FVC% predicted, median (IQR)
79 (67–94)
79 (61–99)
NS
FEV1/FVC% predicted, median (IQR)
77 (73–85)
83 (79–87)
0.09
TLC% predicted, median (IQR)
80 (65–85)
73 (68–88)
NS
Dl
CO_Hb% predicted, median (IQR)
58 (45–70)
37 (25–63)
NS
Admission laboratories
D-dimer, ng/ml, median (IQR)
1,377 (919–1,996)
1,965 (892–4,000)
NS
C-reactive protein, mg/ml, median (IQR)
36.4 (24.8–103.8)
85.0 (56.4–146.5)
NS
Ferritin, ng/ml, median (IQR)
297 (206–506)
701 (314–2,483)
0.02
Troponin, ng/L, median (IQR)
18.0 (7.8–45)
37.0 (20–66)
0.06
Lactate, mmol/L, median (IQR)
1.4 (1.1–1.9)
1.9 (1.6–2.4)
>0.05
IL-6, pg/ml, median (IQR)
23.6 (5.8–216.6)
67.6 (28.5–212.0)
NS
Acute kidney injury, n (%)
6 (30)
7 (47)
NS
Liver function abnormalities, n (%)
7 (39)
8 (57)
NS
Therapies, n (%)
Hydroxychloroquine
4 (13)
6 (40)
0.06
Remdesivir
5 (17)
1 (7)
NS
Tocilizumab
2 (7)
4 (27)
NS
Steroids (new or increased dose)
3 (10)
1 (7)
NS
Outcomes, n (%)
Hospital admission
‡
19 (61)
15 (100)
0.004
ICU level of care
6 (32)
9 (60)
NS
Mechanical ventilation
5 (83)
8 (89)
NS
Length of stay, d
7 (5–14)
6 (5–13)
NS
Venous thromboembolism
3 (9)
3 (20)
NS
Definition of abbreviations: ACEi = angiotensin-converting enzyme inhibitor; ARB = angiotensin
II receptor blocker; BMI = body mass index; COVID-19 = coronavirus disease; Dl
CO_Hb = Dl
CO adjusted for Hb; ILD = interstitial lung disease; IQR = interquartile range; NS = not
significant (P > 0.1); UIP = usual interstitial pneumonitis.
*
Other immunosuppression in the survivor cohort includes mycophenolate mofetil (n = 2;
18%), rituximab (n = 5; 45%), tacrolimus (n = 1; 9%), and other (n = 5; 45%). In the
nonsurvivor cohort, other immunosuppression includes mycophenolate mofetil (n = 2;
29%), rituximab (n = 2; 29%), and other (n = 4; 57%).
†
UIP (definite or probable by computed tomography) included idiopathic pulmonary fibrosis
(n = 6), connective tissue disease–associated UIP (n = 4), and combined pulmonary
fibrosis and emphysema (n = 1). Non-UIP diagnoses included non-UIP connective tissue
disease–associated ILD (n = 10), cryptogenic organizing pneumonia (n = 5), nonspecific
interstitial pneumonitis (n = 3), hypersensitivity pneumonitis (n = 3), non-UIP combined
pulmonary fibrosis and emphysema (n = 2), smoking-associated ILD (n = 2), sarcoidosis
(n = 1), lymphangioleiomyomatosis (n = 1), pleuroparenchymal fibroelastosis (n = 1),
and unclassifiable (n = 7).
‡
The percentages in subgroups were calculated using the parent group (i.e., the denominator
for ICU level of care was hospital admission).
Discussion
In this case–control study, patients with ILD who contracted COVID-19 had a greater
than fourfold increased adjusted odds of death, were more likely to be hospitalized
and require ICU level of care, and were less likely to be discharged, particularly
to the home, compared with a matched cohort of patients with COVID-19 without ILD.
Accordingly, this study suggests that comorbid ILD is a risk factor for poor outcomes
from COVID-19.
We observed increased odds of worse outcomes in patients with COVID-19 with underlying
ILD. One explanation could be their limited pulmonary reserve. Suitably, nonsurvivors
with ILD had a lower diffusion capacity and higher frequency of fibrotic UIP, although
this was not statistically different from survivors. In addition, COVID-19 could lead
to an acute exacerbation of ILD. Though debated, some studies suggest that viral infections
may associate with ILD exacerbations (8). Finally, although the RECOVERY (Randomized
Evaluation of COVID-19 Therapy) trial demonstrated that use of corticosteroids to
treat COVID-19 was beneficial (9), use of chronic immunosuppression to treat underlying
ILD has raised concerns that it may increase risk of disease (4). In our study, although
patients with ILD had significantly increased use of chronic corticosteroids and other
chronic immunosuppression compared with patients without ILD, the increased odds of
death in the ILD cohort remained significantly elevated even after adjustment for
chronic corticosteroid and/or other immunosuppression use. Similarly, frequency of
chronic corticosteroid or other immunosuppression use, though higher in nonsurvivors
compared with survivors, was not statistically associated with death. These results
are consistent with those from previous coronavirus epidemics, notably severe acute
respiratory syndrome and Middle East respiratory syndrome, in which chronic immunosuppression
did not portend worse outcomes (10). Additional studies are needed to further assess
safety of chronic immunosuppression in COVID-19.
Our study had the following limitations: 1) As a case–control study, it is possible
that there are additional confounding variables for which we did not account. 2) Although
our observations suggest that ILD may be an independent risk factor for worse outcomes
from COVID-19, our small sample size limits comprehensive assessments of other risk
factors for poor outcomes within the ILD cohort. 3) Given the limited sensitivity
of real-time PCR for COVID-19, it is possible that we missed additional cases who
were negative by this initial testing modality. Despite this limitation, we had a
high prevalence of COVID-19 in the ILD cohort (15%), although this may be due to confounding
by testing rather than an increased susceptibility given the overlap between ILD and
COVID-19 symptoms. This confounding, however, would tend to bias our data toward the
null by capturing patients with less severe disease. 4) Constrained geographic area
potentially limits the generalizability of our conclusions. Ongoing larger international
studies will help further elucidate the risk factors and outcomes of patients with
ILD and COVID-19.
In summary, in this multicenter case–control study, patients with ILD, particularly
those of advanced age, had increased odds of severe disease and death from COVID-19.
Patients with ILD should be counseled of their increased risk, with an emphasis on
public health measures to prevent infection in this susceptible population.
Related collections
Most cited references8
- Record: found
- Abstract: found
- Article: not found
Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis
- Record: found
- Abstract: found
- Article: found
Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis
Wei-jie Guan, Wen-hua Liang, Yi. Zhao … (2020)

- Record: found
- Abstract: found
- Article: found
Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 — COVID-NET, 14 States, March 1–30, 2020
Shikha Garg, Lindsay Kim, Michael Whitaker … (2020)