- Record: found
- Abstract: found
- Article: found
Neutrophil-to-lymphocyte ratio as a predictive marker of metabolic syndrome
Read this article at
Abstract
Neutrophil-to-lymphocyte ratio (NLR) serves as a strong prognostic indicator for patients suffering from various diseases. Neutrophil activation promotes the recruitment of a number of different cell types that are involved in acute and chronic inflammation and are associated with cancer treatment outcome. Measurement of NLR, an established inflammation marker, is cost-effective, and it is likely that NLR can be used to predict the development of metabolic syndrome (MS) at an early stage. MS scores range from 1 to 5, and an elevated MS score indicates a greater risk for MS. Monitoring NLR can prevent the risk of MS.
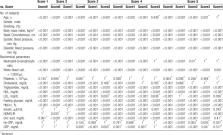
A total of 34,013 subjects were enrolled in this study. The subjects (score 0–5) within the 6 groups were classified according to the National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) criteria, and all anthropometrics, laboratory biomarkers, and hematological measurements were recorded. For the 6 groups, statistical analysis and receiver operating characteristic (ROC) curves were used to identify the development of MS.
Analysis of the ROC curve indicated that NLR served as a good predictor for MS. An MS score of 1 to 2 yielded an acceptable discrimination rate, and these rates were even higher for MS scores of 3 to 5 ( P < .001), where the prevalence of MS was 30.8%.
NLR can be used as a prognostic marker for several diseases, including those associated with MS.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
High preoperative neutrophil-lymphocyte ratio predicts poor survival in patients with gastric cancer.

- Record: found
- Abstract: found
- Article: found