- Record: found
- Abstract: found
- Article: not found
COVID‐19 susceptibility and clinical outcomes in inflammatory bowel disease: An updated systematic review and meta‐analysis

Read this article at
Abstract
The susceptibility, risk factors, and prognosis of COVID‐19 in patients with inflammatory bowel disease (IBD) remain unknown. Thus, our study aims to assess the prevalence and clinical outcomes of COVID‐19 in IBD. We searched PubMed, EMBASE, and medRxiv from 2019 to 1 June 2022 for cohort and case‐control studies comparing the prevalence and clinical outcomes of COVID‐19 in patients with IBD and in the general population. We also compared the outcomes of patients receiving and not receiving 5‐aminosalicylates (ASA), tumour necrosis factor antagonists, biologics, systemic corticosteroids, or immunomodulators for IBD. Thirty five studies were eligible for our analysis. Pooled odds ratio of COVID‐19‐related hospitalisation, intensive care unit (ICU) admission, or death in IBD compared to in non‐IBD were 0.58 (95% confidence interval (CI) = 0.28–1.18), 1.09 (95% CI = 0.27–4.47), and 0.67 (95% CI = 0.32–1.42), respectively. Inflammatory bowel disease was not associated with increased hospitalisation, ICU admission, or death. Susceptibility to COVID‐19 did not increase with any drugs for IBD. Hospitalisation, ICU admission, and death were more likely with 5‐ASA and corticosteroid use. COVID‐19‐related hospitalisation (Odds Ratio (OR): 0.53; 95% CI = 0.38–0.74) and death (OR: 0.13; 95% CI = 0.13–0.70) were less likely with Crohn's disease than ulcerative colitis (UC). In conclusion, IBD does not increase the mortality and morbidity of COVID‐19. However, physicians should be aware that additional monitoring is needed in UC patients or in patients taking 5‐ASA or systemic corticosteroids.
Related collections
Most cited references68
- Record: found
- Abstract: found
- Article: not found
Clinical Characteristics of Coronavirus Disease 2019 in China
- Record: found
- Abstract: found
- Article: found
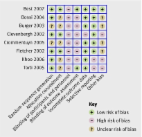
The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials
- Record: found
- Abstract: not found
- Article: not found
