- Record: found
- Abstract: found
- Article: not found
Comparison of pneumonia features in children caused by SARS‐CoV‐2 and other viral respiratory pathogens
Read this article at
Abstract
Background
Pneumonia is a frequent manifestation of coronavirus disease 2019 (COVID‐19) in hospitalized children.
Methods
The study involved 80 hospitals in the severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) Spanish Pediatric National Cohort. Participants were children <18 years, hospitalized with SARS‐CoV‐2 community‐acquired pneumonia (CAP). We compared the clinical and radiological characteristics of SARS‐CoV‐2‐associated CAP with CAP due to other viral etiologies from ValsDance (retrospective) cohort.
Results
In total, 151 children with SARS‐CoV‐2‐associated CAP and 138 with other viral CAP were included. Main clinical features of SARS‐CoV‐2‐associated CAP were cough, fever, or dyspnea. Lymphopenia was found in 43% patients and 15% required admission to the pediatric intensive care unit (PICU). Chest X‐ray revealed condensation (42%) and other infiltrates (58%). Compared with CAP from other viral pathogens, COVID‐19 patients were older, with lower C‐reactive protein (CRP) levels, less wheezing, and greater need of mechanical ventilation (MV). There were no differences in the use of continuous positive airway pressure (CPAP) or HVF, or PICU admission between groups.
Conclusion
SARS‐CoV‐2‐associated CAP in children presents differently to other virus‐associated CAP: children are older and rarely have wheezing or high CRP levels; they need less oxygen but more CPAP or MV. However, several features overlap and differentiating the etiology may be difficult. The overall prognosis is good.
Related collections
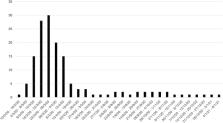
Most cited references40
- Record: found
- Abstract: found
- Article: not found
Clinical Characteristics of Coronavirus Disease 2019 in China
- Record: found
- Abstract: found
- Article: found
Systematic review of COVID‐19 in children shows milder cases and a better prognosis than adults

- Record: found
- Abstract: found
- Article: found
