- Record: found
- Abstract: found
- Article: found
Fatty liver disease in children (MAFLD/PeFLD Type 2): unique classification considerations and challenges
Read this article at
Abstract
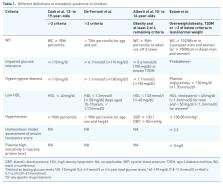
In children, fatty liver disease is a group of disorders that often overlaps with inherited metabolic disorders (IMDs), which requires prompt diagnosis and specific management. Metabolic dysfunction–associated fatty liver disease (MAFLD) or, formerly, non-alcoholic fatty liver disease (NAFLD) is the hepatic component of a multisystemic disease that requires a positive criteria in metabolic dysfunction for diagnosis. However, in children, the diagnosis of MAFLD is one of the exclusions of an IMD [paediatric fatty liver disease (PeFLD) type 1] including the possibility that an IMD can be identified in the future following investigations that may be negative at the time. Therefore, while children with fatty liver with metabolic dysfunction could be classified as MAFLD (PeFLD type 2) and managed that way, those who do not fulfil the criteria for metabolic dysfunction should be considered separately bearing in mind the possibility of identifying a yet undiagnosed IMD (PeFLD type 3). This concept is ever more important in a world where MAFLD is the most common cause of liver disease in children and adolescents in whom about 7% are affected. The disease is only partially understood, and awareness is still lacking outside hepatology and gastroenterology. Despite its increasing pervasiveness, the management is far from a one-size-fits-all. Increasing complexities around the genetic, epigenetic, non-invasive modalities of assessment, psychosocial impacts, therapeutics, and natural history of the disease have meant that an individualised approach is required. This is where the challenge lies so that children with fatty liver are considered on their own merits. The purpose of this review is to give a clinical perspective of fatty liver disease in children with relevance to metabolic dysfunction.
Related collections
Most cited references110
- Record: found
- Abstract: not found
- Article: not found
The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases.
- Record: found
- Abstract: found
- Article: not found
Design and validation of a histological scoring system for nonalcoholic fatty liver disease.
- Record: found
- Abstract: found
- Article: not found