- Record: found
- Abstract: found
- Article: found
A Web-Based Clinical System for Cohort Surveillance of Specific Clinical Effectiveness and Safety Outcomes: A Cohort Study of Non–Vitamin K Antagonist Oral Anticoagulants and Warfarin
Abstract
Background
Conventional systems of drug surveillance lack a seamless workflow, which makes it crucial to have an active drug surveillance system that proactively assesses adverse drug events.
Objective
The aim of this study was to develop a seamless, Web-based workflow for comparing the safety and effectiveness of drugs in a database of electronic medical records.
Methods
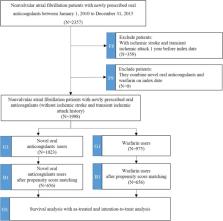
We proposed a comprehensive integration process for cohort surveillance using the National Taiwan University Hospital Clinical Surveillance System (NCSS). We studied a practical application of the NCSS that evaluates the drug safety and effectiveness of novel oral anticoagulants (NOACs) and warfarin by cohort tree analysis in an efficient and interoperable platform.
Results
We demonstrated a practical example of investigating the differences in effectiveness and safety between NOACs and warfarin in patients with nonvalvular atrial fibrillation (AF) using the NCSS. We efficiently identified 2357 patients with nonvalvular AF with newly prescribed oral anticoagulants between 2010 and 2015 and further developed 1 main cohort and 2 subcohorts for separately measuring ischemic stroke as the clinical effectiveness outcome and intracranial hemorrhage (ICH) as the safety outcome. In the subcohort of ischemic stroke, NOAC users exhibited a significantly lower risk of ischemic stroke than warfarin users after adjusting for age, sex, comorbidity, and comedication in an intention-to-treat (ITT) analysis ( P=.01) but did not exhibit a significantly distinct risk in an as-treated (AT) analysis ( P=.12) after the 2-year follow-up. In the subcohort of ICH, NOAC users did not exhibit a different risk of ICH both in ITT ( P=.68) and AT analyses ( P=.15).
Related collections
Most cited references24

- Record: found
- Abstract: found
- Article: found
A comparison of 12 algorithms for matching on the propensity score
- Record: found
- Abstract: found
- Article: not found
Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with atrial fibrillation.
- Record: found
- Abstract: found
- Article: not found