- Record: found
- Abstract: found
- Article: found
Evaluation of Amphetamine-Related Hospitalizations and Associated Clinical Outcomes and Costs in the United States
Read this article at
Key Points
Question
What are the current trends in frequency and costs of amphetamine-related hospitalizations in the United States?
Abstract
Importance
Despite indications of increasing amphetamine availability and psychostimulant deaths in the United States, evidence across data sources is mixed, and data on amphetamine-related hospitalizations are lacking.
Objective
To clarify trends in amphetamine-related hospitalizations and their clinical outcomes and costs in the United States.
Design, Setting, and Participants
This repeated, cross-sectional study used hospital discharge data from the Healthcare Cost and Utilization Project National Inpatient Sample. The nationally representative sample included US adults (n = 1 292 300) who had amphetamine-related hospitalizations between January 1, 2003, and December 31, 2015. Multivariable logistic and Poisson regression models were used to examine in-hospital mortality and length of stay. Analysis of these data was conducted from November 2017 to August 2018.
Main Outcomes and Measures
Annual hospitalizations, in-hospital mortality, length of stay, transfer to another facility, and costs.
Results
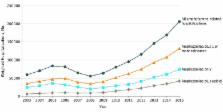
Over the 2003 to 2015 study period, there were 1 292 300 weighted amphetamine-related hospitalizations. Of this population, 541 199 (41.9%) were female and 749 392 (58.1%) were male, with a mean age of 37.5 years (95% CI, 37.4-37.7 years). Amphetamine-related hospitalizations, compared with other hospitalizations, were associated with age younger than 65 years (98.0% vs 58.0%; P < .001), male sex (60.3% [95% CI, 59.7%-60.8%] vs 41.1% [95% CI, 40.9%-41.3%]), Medicaid coverage (51.2% [95% CI, 49.8%-52.7%] vs 17.8% [95% CI, 17.5%-18.1%]), and residence in the western United States (58.5% [95% CI, 55.9%-61.0%] vs 18.9% [95% CI, 18.0%-19.8%]). Amphetamine-related hospitalizations declined between 2005 and 2008, and then increased from 55 447 hospitalizations (95% CI, 44 936-65 959) in 2008 to 206 180 hospitalizations (95% CI, 95% CI, 189 188-223 172) in 2015. Amphetamine-related hospitalizations increased to a greater degree than hospitalizations associated with other substances. Adjusted mean length of stay (5.9 [95% CI, 5.8-6.0] vs 4.7 [95% CI, 4.7-4.8] days; P < .001), transfer to another facility (26.0% [95% CI, 25.3%-26.8%] vs 18.5% [95% CI, 18.3%-18.6%]; P < .001), and mean in-hospital mortality (28.3 [95% CI, 26.2-30.4] vs 21.9 [95% CI, 21.6-22.1] deaths per 1000 hospitalizations; P < .001) were higher for amphetamine-related than other hospitalizations. Annual hospital costs related to amphetamines increased from $436 million (95% CI, $312 million-$559 million) in 2003 to $2.17 billion (95% CI, $1.95 billion-$2.39 billion) by 2015.
Abstract
This cross-sectional study examines Healthcare Cost and Utilization Project National Inpatient Sample data from 2003 to 2015 to identify the frequency, outcomes, and cost of hospitalizations associated with amphetamine use in the United States.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: found
The Prescription Opioid and Heroin Crisis: A Public Health Approach to an Epidemic of Addiction
- Record: found
- Abstract: found
- Article: not found
Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001-2002 to 2012-2013
- Record: found
- Abstract: not found
- Article: not found