- Record: found
- Abstract: found
- Article: found
The effect of smoking status on efficacy of immune checkpoint inhibitors in metastatic non-small cell lung cancer: A systematic review and meta-analysis

Read this article at
Abstract
Background
It remains uncertain whether smoking status can effect efficacy of immune checkpoint inhibitors (ICIs) in metastatic non-small cell lung cancer (NSCLC). We performed a meta-analysis to address this issue.
Patients and methods
PubMed, Embase, Cochrane Library, Web of Science, and international meetings were searched until April 1, 2021, for phase 2 and 3 randomized controlled trials (RCTs) which compared ICIs with chemotherapy (CT) and reported overall survival (OS) and/or progression-free survival (PFS) data according to smoking status. This meta-analysis was registered in INPLASY platform (#INPLASY202140025). The random-effect model was used for statistical analysis.
Findings
Twenty-eight articles from 24 RCTs including 13918 patients were eligible. ICIs significantly prolonged OS than CT in smokers (hazard ratio [HR] = 0.75, 95% confidence interval [CI]: 0.69-0.81), but not in never-smokers (HR = 0.87, 95% CI: 0.74-1.04); while there was no significant treatment-smoking interaction (P interaction = 0.11). Significant heterogeneity was observed for both smokers (OS: I 2 = 60%, P = 0.0002; PFS: I 2 = 74%, P < 0.0001) and never smokers (PFS: I 2 = 69%, P < 0.0001). Subgroup analyses revealed that ICIs monotherapy significantly improved OS in smokers (HR = 0.76, 95% CI: 0.69-0.85) but not in never-smokers (HR = 0.93, 95% CI: 0.77-1.12, P interaction = 0.07), and treatment-smoking interaction was significant in patients with PD-L1 ≥50% (HR, 0.61 vs 1.18; P interaction = 0.005). ICIs plus CT achieved better OS either in smokers or never-smokers (HR, 0.76 vs 0.61; P interaction = 0.39), while dual ICIs combination prolonged OS only in smokers but never-smokers (HR, 0.68 vs 1.02; P interaction = 0.02).
Interpretation
Either ICIs monotherapy or combination therapy was superior to CT in smokers. While ICIs monotherapy and dual ICIs combination were less effective in never-smokers, and ICIs plus CT might be the optimal selection. Nevertheless, given the limitation of the high heterogeneity of studies included, the findings need to be confirmed by future RCTs focusing on this subject.
Related collections
Most cited references51
- Record: found
- Abstract: found
- Article: found
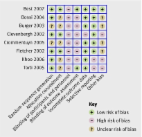
The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials
- Record: found
- Abstract: found
- Article: not found
Pembrolizumab versus Chemotherapy for PD-L1–Positive Non–Small-Cell Lung Cancer
- Record: found
- Abstract: found
- Article: not found
