- Record: found
- Abstract: found
- Article: not found
Effect of the COVID-19 Pandemic on Patient Volumes, Acuity, and Outcomes in Pediatric Emergency Departments : A Nationwide Study

Read this article at
Abstract
Supplemental digital content is available in the text.
Abstract
Objectives
The aim of this study was to quantify the effect of the COVID-19 pandemic on pediatric emergency department (ED) utilization and outcomes.
Methods
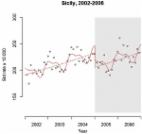
This study is an interrupted-time-series observational study of children presenting to 11 Canadian tertiary-care pediatric EDs. Data were grouped into weeks in 3 study periods: prepandemic (January 1, 2018–January 27, 2020), peripandemic (January 28, 2020–March 10, 2020), and early pandemic (March 11, 2020–April 30, 2020). These periods were compared with the same time intervals in the 2 preceding calendar years. Primary outcomes were number of ED visits per week. The secondary outcomes were triage acuity, hospitalization, intensive care unit (ICU) admission, mortality, length of hospital stay, ED revisits, and visits for trauma and mental health concerns.
Results
There were 577,807 ED visits (median age, 4.5 years; 52.9% male). Relative to the prepandemic period, there was a reduction [−58%; 95% confidence interval (CI), −63% to −51%] in the number of ED visits during the early-pandemic period, with concomitant higher acuity. There was a concurrent increase in the proportion of ward [odds ratio (OR), 1.39; 95% CI, 1.32–1.45] and intensive care unit (OR, 1.20; 95% CI, 1.01–1.42) admissions, and trauma-related ED visits among children less than 10 years (OR, 1.51; 95% CI, 1.45–1.56). Mental health–related visits in children declined in the early-pandemic period (in <10 years, −60%; 95% CI, −67% to −51%; in children ≥10 years: −56%; 95% CI, −63% to −47%) relative to the pre–COVID-19 period. There were no differences in mortality or length of stay; however, ED revisits within 72 hours were reduced during the early-pandemic period (percent change: −55%; 95% CI, −61% to −49%; P < 0.001).
Conclusions
After the declaration of the COVID-19 pandemic, dramatic reductions in pediatric ED visits occurred across Canada. Children seeking ED care were sicker, and there was an increase in trauma-related visits among children more than 10 years of age, whereas mental health visits declined during the early-pandemic period. When faced with a future pandemic, public health officials must consider the impact of the illness and the measures implemented on children's health and acute care needs.
Related collections
Most cited references41
- Record: found
- Abstract: found
- Article: not found
The outbreak of COVID-19 coronavirus and its impact on global mental health
- Record: found
- Abstract: found
- Article: found
Interrupted time series regression for the evaluation of public health interventions: a tutorial
- Record: found
- Abstract: found
- Article: not found
