- Record: found
- Abstract: found
- Article: found
Robotic Abdominal Surgery and COVID-19: A Systematic Review of Published Literature and Peer-Reviewed Guidelines during the SARS-CoV-2 Pandemic
Read this article at
Abstract
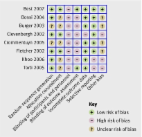
Background: Significant concern emerged at the beginning of the SARS-CoV-2 pandemic regarding the safety and practicality of robotic-assisted surgery (RAS). We aimed to review reported surgical practice and peer-reviewed published review recommendations and guidelines relating to RAS during the pandemic. Methods: A systematic review was performed in keeping with PRISMA guidelines. This study was registered on Open Science Framework. Databases were searched using the following search terms: ‘robotic surgery’, ‘robotics’, ‘COVID-19’, and ‘SARS-CoV-2’. Firstly, articles describing any outcome from or reference to robotic surgery during the COVID-19/SARS-CoV-2 pandemic were considered for inclusion. Guidelines or review articles that outlined recommendations were included if published in a peer-reviewed journal and incorporating direct reference to RAS practice during the pandemic. The ROBINS-I (Risk of Bias in Non-Randomised Studies of Intervention) tool was used to assess the quality of surgical practice articles and guidelines and recommendation publications were assessed using the AGREE-II reporting tool. Publication trends, median time from submission to acceptance were reported along with clinical outcomes and practice recommendations. Results: Twenty-nine articles were included: 15 reporting RAS practice and 14 comprising peer-reviewed guidelines or review recommendations related to RAS during the pandemic, with multiple specialities (i.e., urology, colorectal, digestive surgery, and general minimally invasive surgery) covered. Included articles were published April 2020—December 2021, and the median interval from first submission to acceptance was 92 days. All surgical practice studies scored ‘low’ or ‘moderate’ risk of bias on the ROBINS-I assessment. All guidelines and recommendations scored ‘moderately well’ on the AGREE-II assessment; however, all underperformed in the domain of public and patient involvement. Overall, there were no increases in perioperative complication rates or mortalities in patients who underwent RAS compared to that expected in non-COVID practice. RAS was deemed safe, with recommendations for mitigation of risk of viral transmission. Conclusions: Continuation of RAS was feasible and safe during the SARS-CoV-2 pandemic where resources permitted. Post-pandemic reflections upon published robotic data and publication patterns allows us to better prepare for future events and to enhance urgent guideline design processes.
Related collections
Most cited references44
- Record: found
- Abstract: found
- Article: found
The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials
- Record: found
- Abstract: found
- Article: found
Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement

- Record: found
- Abstract: found
- Article: found