- Record: found
- Abstract: found
- Article: found
Post Herpetic Neuralgia: A Retrospective Study to Evaluate Response to Modified Jaipur Block with Increased Concentration of Dexamethasone
Read this article at
Abstract
Background:
Postherpetic neuralgia (PHN) is a complication of herpes zoster characterized by persistent dermatomal pain. It has a negative impact on the quality of life. There is no gold standard therapy for PHN, and various local and systemic treatments have been tried. There are studies reporting the use of combination of steroids and local anesthetics but there is no standardized method.
Aim:
To evaluate the response of modified Jaipur block with increased concentration of dexamethasone.
Methods:
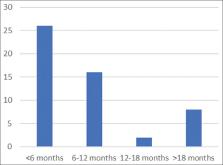
We conducted a retrospective study in patients who were given Jaipur block. The patients age, sex, duration of PHN, type and severity of pain were observed. A combination of 2% lignocaine and 0.5% bupivacaine and dexamethasone was injected subcutaneously. The pain was scored using visual analogue scale at the baseline, and 1 month after 1 st, 2 nd, and 3 rd session of block and follow up after 6 months and 1 year.
Results:
The mean age of our patient was 63.33 ± 9.5 years. The males outnumbered females. Thoracic dermatomes were more commonly involved. The mean duration of PHN was 11.58 ± 12.76 months; stimulus evoked PHN was the commonest type of pain seen. The mean visual analogue score (VAS) decreased progressively after each session of the block. Maximum patients (50%) had excellent response, whereas 1.9% did not respond to the block. Relapse of pain was seen in 5.6% of the patients. There was no significant side effect noted.
Related collections
Most cited references24
- Record: found
- Abstract: found
- Article: not found
Postherpetic neuralgia: irritable nociceptors and deafferentation.
- Record: found
- Abstract: found
- Article: not found
Corticosteroids suppress ectopic neural discharge originating in experimental neuromas.
- Record: found
- Abstract: found
- Article: not found