- Record: found
- Abstract: found
- Article: found
Early impact of COVID-19 social distancing measures on reported sexual behaviour of HIV pre-exposure prophylaxis users in Wales
Read this article at
Abstract
Objectives
To describe the early impact of COVID-19 and associated control measures on the sexual behaviour of pre-exposure prophylaxis (PrEP) users in Wales.
Methods
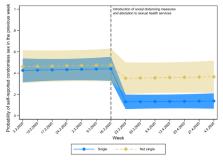
Data were obtained from an ecological momentary assessment study of PrEP use and sexual behaviour. Participants were individuals accessing PrEP through the National Health Service (NHS) sexual health clinics across four health boards in Wales. Weekly data documenting condomless sex in the preceding week were analysed between 03/02/2020 and 10/05/2020. The introduction of social distancing measures and changes to sexual health clinics in Wales occurred on the week starting 16/03/2020. Two-level logistic regression models were fitted to condomless sex (yes/no) over time, included an indicator for the week starting 16/03/2020, and were extended to explore differential associations by relationship status and sexual health clinic.
Results
Data were available from 56 participants and included 697 person-weeks (89% of the maximum number that could have been obtained). On average, 42% of participants reported condomless sex in the period prior to the introduction of social distancing measures and 20% reported condomless sex after (OR=0.16, 95% CI 0.07 to 0.37, p<0.001). There was some evidence to suggest that this association was moderated by relationship status (OR for single participants=0.09, 95% CI 0.06 to 0.23; OR for not single participants=0.46, 95% CI 0.16 to 1.25).
Conclusions
The introduction of social distancing measures and changes to PrEP services across Wales was associated with a marked reduction in reported instances of condomless sexual intercourse among respondents, with a larger reduction in those who were single compared with those who were not. The long-term impact of COVID-19 and associated control measures on this population’s physical and mental health and well-being requires close examination.
Related collections
Most cited references4
- Record: found
- Abstract: found
- Article: not found
Preexposure Chemoprophylaxis for HIV Prevention in Men Who Have Sex with Men
- Record: found
- Abstract: not found
- Article: not found
Ecological Momentary Assessment (Ema) in Behavioral Medicine
- Record: found
- Abstract: found
- Article: not found