- Record: found
- Abstract: found
- Article: found
Using the Clinical Frailty Scale in Allocating Scarce Health Care Resources
Read this article at
Abstract
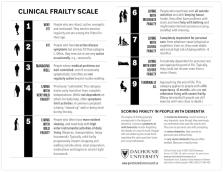
The key idea behind the Clinical Frailty Scale (CFS) is that, as people age, they are more likely to have things wrong with them. Those things they have wrong (health deficits) can, as they accumulate, erode their ability to do the high order functions which define their overall health. These high order functions include being able to: think and do as they please; look after themselves; interact with other people; and move about without falling. The Clinical Frailty Scale brings that information together in one place. This paper is a guide for people new to the Clinical Frailty Scale. It also introduces an updated version (CFS version 2.0), with revised level names (e.g., “vulnerable” becomes “living with very mild frailty”) and minor edits to level descriptions. The key points discussed are that the Clinical Frailty Scale assays the baseline state, it is not widely validated in younger people or those with stable single-system disabilities, and it requires clinical judgement. The Clinical Frailty Scale is now commonly used as a triage tool to make important clinical decisions such as allocating scarce health care resources for COVID-19 management; therefore, it is important that the scale is used appropriately.
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Covid-19 in Critically Ill Patients in the Seattle Region — Case Series
- Record: found
- Abstract: not found
- Article: not found
Age-related deficit accumulation and the diseases of ageing
- Record: found
- Abstract: found
- Article: not found