- Record: found
- Abstract: found
- Article: found
Mechanisms linking childhood trauma exposure and psychopathology: a transdiagnostic model of risk and resilience
Read this article at
Abstract
Background
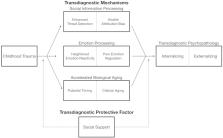
Transdiagnostic processes confer risk for multiple types of psychopathology and explain the co-occurrence of different disorders. For this reason, transdiagnostic processes provide ideal targets for early intervention and treatment. Childhood trauma exposure is associated with elevated risk for virtually all commonly occurring forms of psychopathology. We articulate a transdiagnostic model of the developmental mechanisms that explain the strong links between childhood trauma and psychopathology as well as protective factors that promote resilience against multiple forms of psychopathology.
Main body
We present a model of transdiagnostic mechanisms spanning three broad domains: social information processing, emotional processing, and accelerated biological aging. Changes in social information processing that prioritize threat-related information—such as heightened perceptual sensitivity to threat, misclassification of negative and neutral emotions as anger, and attention biases towards threat-related cues—have been consistently observed in children who have experienced trauma. Patterns of emotional processing common in children exposed to trauma include elevated emotional reactivity to threat-related stimuli, low emotional awareness, and difficulties with emotional learning and emotion regulation. More recently, a pattern of accelerated aging across multiple biological metrics, including pubertal development and cellular aging, has been found in trauma-exposed children. Although these changes in social information processing, emotional responding, and the pace of biological aging reflect developmental adaptations that may promote safety and provide other benefits for children raised in dangerous environments, they have been consistently associated with the emergence of multiple forms of internalizing and externalizing psychopathology and explain the link between childhood trauma exposure and transdiagnostic psychopathology. Children with higher levels of social support, particularly from caregivers, are less likely to develop psychopathology following trauma exposure. Caregiver buffering of threat-related processing may be one mechanism explaining this protective effect.
Conclusion
Childhood trauma exposure is a powerful transdiagnostic risk factor associated with elevated risk for multiple forms of psychopathology across development. Changes in threat-related social and emotional processing and accelerated biological aging serve as transdiagnostic mechanisms linking childhood trauma with psychopathology. These transdiagnostic mechanisms represent critical targets for early interventions aimed at preventing the emergence of psychopathology in children who have experienced trauma.
Related collections
Most cited references111
- Record: found
- Abstract: not found
- Article: not found
Stress, social support, and the buffering hypothesis.
- Record: found
- Abstract: found
- Article: not found
Adverse childhood experiences and the risk of depressive disorders in adulthood.
- Record: found
- Abstract: found
- Article: not found