- Record: found
- Abstract: found
- Article: found
Interpretation of Negative Molecular Test Results in Patients With Suspected or Confirmed Ebola Virus Disease: Report of Two Cases
Read this article at
Abstract
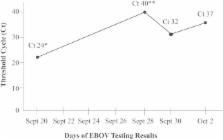
Quantitative reverse-transcription polymerase chain reaction (qRT-PCR) is the most sensitive quantitative diagnostic assay for detection of Ebola virus in multiple body fluids. Despite the strengths of this assay, we present 2 cases of Ebola virus disease (EVD) and highlight the potential for false-negative results during the early and late stages of EVD. The first case emphasizes the low negative-predictive value of qRT-PCR during incubation and the early febrile stage of EVD, and the second case emphasizes the potential for false-negative results during recovery and late neurologic complications of EVD. Careful interpretation of test results are needed to guide difficult admission and discharge decisions in suspected or confirmed EVD.
Related collections
Most cited references6
- Record: found
- Abstract: not found
- Article: not found
Ebola virus disease in West Africa--clinical manifestations and management.
- Record: found
- Abstract: found
- Article: not found