- Record: found
- Abstract: found
- Article: found
Health policy considerations for combining exercise prescription into noncommunicable diseases treatment: a narrative literature review
Read this article at
Abstract
Objectives
In this review, we aim to highlight the evidence base for the benefits of exercise in relation to the treatment of noncommunicable diseases (NCDs), draw on the Health Triangular Policy Framework to outline the principal facilitators and barriers for implementing exercise in health policy, and make concrete suggestions for action.
Methods
Literature review and framework analysis were conducted to deal with the research questions.
Results
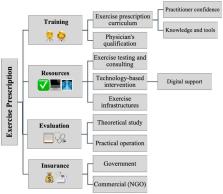
Exercise prescription is a safe solution for noncommunicable diseases prevention and treatment that enables physicians to provide and instruct patients how to apply exercise as an important aspect of disease treatment and management. Combining exercise prescription within routine care, in inpatient and outpatient settings, will improve patients’ life quality and fitness levels.
Conclusion
Inserting exercise prescription into the healthcare system would improve population health status and healthy lifestyles. The suggestions outlined in this study need combined efforts from the medical profession, governments, and policymakers to facilitate practice into reality in the healthcare arena.
Related collections
Most cited references71
- Record: found
- Abstract: found
- Article: not found
Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases.
- Record: found
- Abstract: found
- Article: not found
NCD Countdown 2030: worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4
- Record: found
- Abstract: found
- Article: not found