- Record: found
- Abstract: found
- Article: found
The negative association of the SARS-CoV-2 pandemic with the health of mother and child considering maternal childhood maltreatment
Read this article at
Abstract
Background
Social distancing strategies during the SARS-CoV-2 pandemic have left families facing a variety of different constraints. Especially in this stressful time, children need a stable parental home to prevent developmental consequences. Additional risk factors such as maternal childhood maltreatment (CM) may affect mother’s psychosomatic health and children’s physical well-being in this period.
Objective
It was aimed to analyze the associations between maternal CM, mother’s mental health, and children’s physical complaints during the SARS-CoV-2-pandemic.
Method
Mothers of a well-documented birth cohort from a longitudinal study were included in this study. Psychosomatic health was assessed with the PHQ-D and children’s physical health with the GBB-KJ during the pandemic. N = 159 mothers completed the online survey. To describe the maternal CM, data from a longitudinal survey were used.
Results
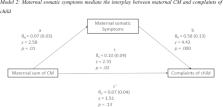
The calculation of three mediation analyses demonstrate that maternal depression symptoms (c-path: β = 0.10, p = .02; c’-path: β = 0.07, p = .13), somatic symptoms (c-path: β = 0.10, p = .02; c’-path: β = 0.07, p = .13) and psychosomatic symptoms (c-path: β = 0.10, p = .02; c’-path: β = 0.06, p = .19) fully mediate the relationship between CM and children’s physical health complaints.
Conclusions
Maternal CM experiences seem to be one relevant risk factor during the pandemic and seem to influence the way in which parents deal with stressful situations and increase the risk for depressive symptoms. The present results highlight the importance to provide individually adjusted assistance to help the families to get through the pandemic.
Related collections
Most cited references59
- Record: found
- Abstract: found
- Article: found
Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China
- Record: found
- Abstract: not found
- Article: not found
lavaan: AnRPackage for Structural Equation Modeling
- Record: found
- Abstract: found
- Article: not found