- Record: found
- Abstract: found
- Article: found
Graphene oxide as an interface phase between polyetheretherketone and hydroxyapatite for tissue engineering scaffolds

Read this article at
Abstract
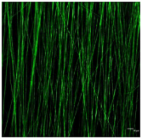
The poor bonding strength between biopolymer and bioceramic has remained an unsolved issue. In this study, graphene oxide (GO) was introduced as an interface phase to improve the interfacial bonding between polyetheretherketone (PEEK) and hydroxyapatite (HAP) for tissue engineering scaffolds. On the one hand, the conjugated structure of GO could form strong π-π stacking interaction with the benzene rings in PEEK. On the other hand, GO with a negatively charge resulting from oxygen functional groups could adsorb the positively charged calcium atoms (C sites) of HAP. Consequently, the dispersibility and compatibility of HAP in the PEEK matrix increased with increasing GO content up to 1 wt%. At this time, the compressive strength and modulus of scaffolds increased by 79.45% and 42.07%, respectively. Furthermore, the PEEK-HAP with GO (PEEK-HAP/GO) scaffolds possessed the ability to induce formation of bone-like apatite. And they could support cellular adhesion, proliferation as well as osteogenic differentiation. More importantly, in vivo bone defect repair experiments showed that new bone formed throughout the scaffolds at 60 days after implantation. All these results suggested that the PEEK-HAP/GO scaffolds have a promising potential for bone tissue engineering application.
Related collections
Most cited references63
- Record: found
- Abstract: found
- Article: not found
Recent advances in bone tissue engineering scaffolds.
- Record: found
- Abstract: found
- Article: found
An Overview of Poly(lactic-co-glycolic) Acid (PLGA)-Based Biomaterials for Bone Tissue Engineering
- Record: found
- Abstract: found
- Article: not found