- Record: found
- Abstract: found
- Article: found
Factors associated with relapse into drug use among male and female attendees of a three-month drug detoxification–rehabilitation programme in Dhaka, Bangladesh: a prospective cohort study
Read this article at
Abstract
Background
To determine relapse rates and associated factors among people who use drugs (PWUDs) attending abstinence-oriented drug treatment clinics in Dhaka, Bangladesh.
Methods
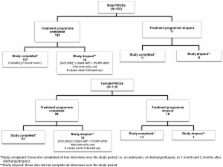
A cohort of male and female PWUDs admitted to the 3-month drug detoxification-rehabilitation treatment programmes of three non-governmental organisation-run drug treatment clinics in Dhaka, Bangladesh were interviewed on admission and over the following 5 months, which included the first 2 months after discharge. The study subjects comprised 150 male and 110 female PWUDs who had been taking opiates/opioids, cannabis or other drugs (including sedatives) before admission, had provided informed consent and were aged ≥16 years. Interviews were conducted using semi-structured questionnaires at four time points; on admission, at discharge and at 1 and 2 months after discharge. Relapse rates were assessed by the Kaplan–Meier method. Factors associated with relapse on enrolment and after discharge were determined using the Cox proportional hazards regression model.
Results
A greater proportion of female than male subjects relapsed over the study period (71.9% versus 54.5%, p < 0.01). For men, baseline factors associated with relapse were living with other PWUDs (relative hazard ratio [RHR] = 2.27), living alone (RHR = 2.35) and not having sex with non-commercial partners (RHR = 2.27); whereas for women these were previous history of drug treatment (RHR = 1.94), unstable housing (RHR = 2.44), higher earnings (RHR = 1.89), preferring to smoke heroin (RHR = 3.62) and injecting buprenorphine/pethidine (RHR = 3.00). After discharge, relapse for men was associated with unstable housing (RHR = 2.78), living alone (RHR = 3.69), higher earnings (RHR = 2.48) and buying sex from sex workers (RHR = 2.29). Women’ relapses were associated with not having children to support (RHR = 3.24) and selling sex (RHR = 2.56).
Conclusions
The relapse rate was higher for female PWUDs. For both male and female subjects the findings highlight the importance of stable living conditions. Additionally, female PWUDs need gender-sensitive services and active efforts to refer them for opioid substitution therapy, which should not be restricted only to people who inject drugs.
Related collections
Most cited references11
- Record: found
- Abstract: found
- Article: not found
Prediction of relapse to frequent heroin use and the role of methadone prescription: an analysis of the Amsterdam Cohort Study among drug users.
- Record: found
- Abstract: not found
- Article: not found
Science-based views of drug addiction and its treatment.
- Record: found
- Abstract: found
- Article: not found