- Record: found
- Abstract: not found
- Article: not found
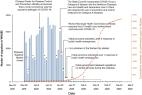
Reopening dentistry after COVID-19: Complete suppression of aerosolization in dental procedures by viscoelastic Medusa Gorgo
Author(s):
Jevon Plog
1 ,
Jingwei Wu
1 ,
Yasmin J. Dias
1 ,
Farzad Mashayek
1 ,
Lyndon F. Cooper
2 ,
Alexander L. Yarin
1
Publication date Created:
August 01 2020
Publication date (Print):
August 01 2020
Journal:
Physics of Fluids
Publisher:
AIP Publishing
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1
To the Editor: A novel human coronavirus that is now named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (formerly called HCoV-19) emerged in Wuhan, China, in late 2019 and is now causing a pandemic. 1 We analyzed the aerosol and surface stability of SARS-CoV-2 and compared it with SARS-CoV-1, the most closely related human coronavirus. 2 We evaluated the stability of SARS-CoV-2 and SARS-CoV-1 in aerosols and on various surfaces and estimated their decay rates using a Bayesian regression model (see the Methods section in the Supplementary Appendix, available with the full text of this letter at NEJM.org). SARS-CoV-2 nCoV-WA1-2020 (MN985325.1) and SARS-CoV-1 Tor2 (AY274119.3) were the strains used. Aerosols (<5 μm) containing SARS-CoV-2 (105.25 50% tissue-culture infectious dose [TCID50] per milliliter) or SARS-CoV-1 (106.75-7.00 TCID50 per milliliter) were generated with the use of a three-jet Collison nebulizer and fed into a Goldberg drum to create an aerosolized environment. The inoculum resulted in cycle-threshold values between 20 and 22, similar to those observed in samples obtained from the upper and lower respiratory tract in humans. Our data consisted of 10 experimental conditions involving two viruses (SARS-CoV-2 and SARS-CoV-1) in five environmental conditions (aerosols, plastic, stainless steel, copper, and cardboard). All experimental measurements are reported as means across three replicates. SARS-CoV-2 remained viable in aerosols throughout the duration of our experiment (3 hours), with a reduction in infectious titer from 103.5 to 102.7 TCID50 per liter of air. This reduction was similar to that observed with SARS-CoV-1, from 104.3 to 103.5 TCID50 per milliliter (Figure 1A). SARS-CoV-2 was more stable on plastic and stainless steel than on copper and cardboard, and viable virus was detected up to 72 hours after application to these surfaces (Figure 1A), although the virus titer was greatly reduced (from 103.7 to 100.6 TCID50 per milliliter of medium after 72 hours on plastic and from 103.7 to 100.6 TCID50 per milliliter after 48 hours on stainless steel). The stability kinetics of SARS-CoV-1 were similar (from 103.4 to 100.7 TCID50 per milliliter after 72 hours on plastic and from 103.6 to 100.6 TCID50 per milliliter after 48 hours on stainless steel). On copper, no viable SARS-CoV-2 was measured after 4 hours and no viable SARS-CoV-1 was measured after 8 hours. On cardboard, no viable SARS-CoV-2 was measured after 24 hours and no viable SARS-CoV-1 was measured after 8 hours (Figure 1A). Both viruses had an exponential decay in virus titer across all experimental conditions, as indicated by a linear decrease in the log10TCID50 per liter of air or milliliter of medium over time (Figure 1B). The half-lives of SARS-CoV-2 and SARS-CoV-1 were similar in aerosols, with median estimates of approximately 1.1 to 1.2 hours and 95% credible intervals of 0.64 to 2.64 for SARS-CoV-2 and 0.78 to 2.43 for SARS-CoV-1 (Figure 1C, and Table S1 in the Supplementary Appendix). The half-lives of the two viruses were also similar on copper. On cardboard, the half-life of SARS-CoV-2 was longer than that of SARS-CoV-1. The longest viability of both viruses was on stainless steel and plastic; the estimated median half-life of SARS-CoV-2 was approximately 5.6 hours on stainless steel and 6.8 hours on plastic (Figure 1C). Estimated differences in the half-lives of the two viruses were small except for those on cardboard (Figure 1C). Individual replicate data were noticeably “noisier” (i.e., there was more variation in the experiment, resulting in a larger standard error) for cardboard than for other surfaces (Fig. S1 through S5), so we advise caution in interpreting this result. We found that the stability of SARS-CoV-2 was similar to that of SARS-CoV-1 under the experimental circumstances tested. This indicates that differences in the epidemiologic characteristics of these viruses probably arise from other factors, including high viral loads in the upper respiratory tract and the potential for persons infected with SARS-CoV-2 to shed and transmit the virus while asymptomatic. 3,4 Our results indicate that aerosol and fomite transmission of SARS-CoV-2 is plausible, since the virus can remain viable and infectious in aerosols for hours and on surfaces up to days (depending on the inoculum shed). These findings echo those with SARS-CoV-1, in which these forms of transmission were associated with nosocomial spread and super-spreading events, 5 and they provide information for pandemic mitigation efforts.
- Record: found
- Abstract: found
- Article: found
Coronavirus Disease 2019 (COVID-19): Emerging and Future Challenges for Dental and Oral Medicine
The epidemic of coronavirus disease 2019 (COVID-19), originating in Wuhan, China, has become a major public health challenge for not only China but also countries around the world. The World Health Organization announced that the outbreaks of the novel coronavirus have constituted a public health emergency of international concern. As of February 26, 2020, COVID-19 has been recognized in 34 countries, with a total of 80,239 laboratory-confirmed cases and 2,700 deaths. Infection control measures are necessary to prevent the virus from further spreading and to help control the epidemic situation. Due to the characteristics of dental settings, the risk of cross infection can be high between patients and dental practitioners. For dental practices and hospitals in areas that are (potentially) affected with COVID-19, strict and effective infection control protocols are urgently needed. This article, based on our experience and relevant guidelines and research, introduces essential knowledge about COVID-19 and nosocomial infection in dental settings and provides recommended management protocols for dental practitioners and students in (potentially) affected areas.
- Record: found
- Abstract: found
- Article: not found
Asymptomatic Transmission, the Achilles’ Heel of Current Strategies to Control Covid-19
Monica Gandhi, Deborah S. Yokoe, Diane Havlir (2020)
Traditional infection-control and public health strategies rely heavily on early detection of disease to contain spread. When Covid-19 burst onto the global scene, public health officials initially deployed interventions that were used to control severe acute respiratory syndrome (SARS) in 2003, including symptom-based case detection and subsequent testing to guide isolation and quarantine. This initial approach was justified by the many similarities between SARS-CoV-1 and SARS-CoV-2, including high genetic relatedness, transmission primarily through respiratory droplets, and the frequency of lower respiratory symptoms (fever, cough, and shortness of breath) with both infections developing a median of 5 days after exposure. However, despite the deployment of similar control interventions, the trajectories of the two epidemics have veered in dramatically different directions. Within 8 months, SARS was controlled after SARS-CoV-1 had infected approximately 8100 persons in limited geographic areas. Within 5 months, SARS-CoV-2 has infected more than 2.6 million people and continues to spread rapidly around the world. What explains these differences in transmission and spread? A key factor in the transmissibility of Covid-19 is the high level of SARS-CoV-2 shedding in the upper respiratory tract, 1 even among presymptomatic patients, which distinguishes it from SARS-CoV-1, where replication occurs mainly in the lower respiratory tract. 2 Viral loads with SARS-CoV-1, which are associated with symptom onset, peak a median of 5 days later than viral loads with SARS-CoV-2, which makes symptom-based detection of infection more effective in the case of SARS CoV-1. 3 With influenza, persons with asymptomatic disease generally have lower quantitative viral loads in secretions from the upper respiratory tract than from the lower respiratory tract and a shorter duration of viral shedding than persons with symptoms, 4 which decreases the risk of transmission from paucisymptomatic persons (i.e., those with few symptoms). Arons et al. now report in the Journal an outbreak of Covid-19 in a skilled nursing facility in Washington State where a health care provider who was working while symptomatic tested positive for infection with SARS-CoV-2 on March 1, 2020. 5 Residents of the facility were then offered two facility-wide point-prevalence screenings for SARS-CoV-2 by real-time reverse-transcriptase polymerase chain reaction (rRT-PCR) of nasopharyngeal swabs on March 13 and March 19–20, along with collection of information on symptoms the residents recalled having had over the preceding 14 days. Symptoms were classified into typical (fever, cough, and shortness of breath), atypical, and none. Among 76 residents in the point-prevalence surveys, 48 (63%) had positive rRT-PCR results, with 27 (56%) essentially asymptomatic, although symptoms subsequently developed in 24 of these residents (within a median of 4 days) and they were reclassified as presymptomatic. Quantitative SARS-CoV-2 viral loads were similarly high in the four symptom groups (residents with typical symptoms, those with atypical symptoms, those who were presymptomatic, and those who remained asymptomatic). It is notable that 17 of 24 specimens (71%) from presymptomatic persons had viable virus by culture 1 to 6 days before the development of symptoms. Finally, the mortality from Covid-19 in this facility was high; of 57 residents who tested positive, 15 (26%) died. An important finding of this report is that more than half the residents of this skilled nursing facility (27 of 48) who had positive tests were asymptomatic at testing. Moreover, live coronavirus clearly sheds at high concentrations from the nasal cavity even before symptom development. Although the investigators were not able to retrospectively elucidate specific person-to-person transmission events and although symptom ascertainment may be unreliable in a group in which more than half the residents had cognitive impairment, these results indicate that asymptomatic persons are playing a major role in the transmission of SARS-CoV-2. Symptom-based screening alone failed to detect a high proportion of infectious cases and was not enough to control transmission in this setting. The high mortality (>25%) argues that we need to change our current approach for skilled nursing facilities in order to protect vulnerable, enclosed populations until other preventive measures, such as a vaccine or chemoprophylaxis, are available. A new approach that expands Covid-19 testing to include asymptomatic persons residing or working in skilled nursing facilities needs to be implemented now. Despite “lockdowns” in these facilities, coronavirus outbreaks continue to spread, with 1 in 10 nursing homes in the United States (>1300 skilled nursing facilities) now reporting cases, with the likelihood of thousands of deaths. 6 Mass testing of the residents in skilled nursing facilities will allow appropriate isolation of infected residents so that they can be cared for and quarantine of exposed residents to minimize the risk of spread. Mass testing in these facilities could also allow cohorting 7 and some resumption of group activities in a nonoutbreak setting. Routine rRT-PCR testing in addition to symptomatic screening of new residents before entry, conservative guidelines for discontinuation of isolation, 7 and periodic retesting of long-term residents, as well as both periodic rRT-PCR screening and surgical masking of all staff, are important concomitant measures. There are approximately 1.3 million Americans currently residing in nursing homes. 8 Although this recommendation for mass testing in skilled nursing facilities could be initially rolled out in geographic areas with high rates of community Covid-19 transmission, an argument can be made to extend this recommendation to all U.S.-based skilled nursing facilities now because case ascertainment is uneven and incomplete and because of the devastating consequences of outbreaks. Immediately enforceable alternatives to mass testing in skilled nursing facilities are few. The public health director of Los Angeles has recommended that families remove their loved ones from nursing homes, 9 a measure that is not feasible for many families. Asymptomatic transmission of SARS-CoV-2 is the Achilles’ heel of Covid-19 pandemic control through the public health strategies we have currently deployed. Symptom-based screening has utility, but epidemiologic evaluations of Covid-19 outbreaks within skilled nursing facilities such as the one described by Arons et al. strongly demonstrate that our current approaches are inadequate. This recommendation for SARS-CoV-2 testing of asymptomatic persons in skilled nursing facilities should most likely be expanded to other congregate living situations, such as prisons and jails (where outbreaks in the United States, whose incarceration rate is much higher than rates in other countries, are increasing), enclosed mental health facilities, and homeless shelters, and to hospitalized inpatients. Current U.S. testing capability must increase immediately for this strategy to be implemented. Ultimately, the rapid spread of Covid-19 across the United States and the globe, the clear evidence of SARS-CoV-2 transmission from asymptomatic persons, 5 and the eventual need to relax current social distancing practices argue for broadened SARS-CoV-2 testing to include asymptomatic persons in prioritized settings. These factors also support the case for the general public to use face masks 10 when in crowded outdoor or indoor spaces. This unprecedented pandemic calls for unprecedented measures to achieve its ultimate defeat.
Author and article information
Contributors
Jevon Plog:
(View ORCID Profile)
Jingwei Wu:
(View ORCID Profile)
Yasmin J. Dias:
(View ORCID Profile)
Farzad Mashayek:
(View ORCID Profile)
Lyndon F. Cooper:
(View ORCID Profile)
Alexander L. Yarin:
(View ORCID Profile)
Journal
Title:
Physics of Fluids
Abbreviated Title:
Physics of Fluids
Publisher:
AIP Publishing
ISSN
(Print):
1070-6631
ISSN
(Electronic):
1089-7666
Publication date Created:
August
01 2020
Publication date
(Print):
August
01 2020
Volume: 32
Issue: 8
Page: 083111
Affiliations
Article
DOI: 10.1063/5.0021476
SO-VID: 7655f25b-99f7-4389-a1ad-6de99c8810bc
Copyright © ©
2020
History
Data availability:
