- Record: found
- Abstract: found
- Article: found
Health Disparities in COVID-19: Addressing the Role of Social Determinants of Health in Immune System Dysfunction to Turn the Tide
Read this article at
Abstract
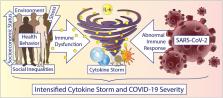
It is evident that health disparities exist during the COVID-19 pandemic, a pandemic caused by the novel coronavirus SARS-CoV-2. Underlying reasons for COVID-19 health disparities are multi-factorial. However, social determinants, including those regarding socioeconomic status, social inequalities, health behaviors, and stress, may have implications on these disparities. Exposure to one or more of these social determinants is associated with heightened inflammatory responses, particularly increases in the cytokine interleukin-6 (IL-6), as well as immune system dysfunction. Thus, an amplified effect during COVID-19 could occur, potentially resulting in vulnerable patients experiencing an intensified cytokine storm due to a hyperactive and dysfunctional immune response. Further understanding how social determinants play a mechanistic role in COVID-19 disparities could potentially help reduce health disparities overall and in future pandemics.
Related collections
Most cited references126

- Record: found
- Abstract: found
- Article: found
OpenSAFELY: factors associated with COVID-19 death in 17 million patients
- Record: found
- Abstract: found
- Article: not found
Clinical and immunologic features in severe and moderate Coronavirus Disease 2019

- Record: found
- Abstract: found
- Article: found