- Record: found
- Abstract: found
- Article: found
Racial-ethnic, gender identity, and sexual orientation disparities in COVID-19-related social and health outcomes: A decomposition analysis

Read this article at
Abstract
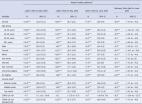
Despite the growing literature on racial-ethnic disparities during the pandemic, less is known about the explanatory mechanisms of these disparities and inequalities across other axes, such as gender and sexual identities. We studied the levels and sources of racial-ethnic, gender identity, and sexual minority disparities in social (i.e., unmet resource needs) and health (i.e., hospitalization) outcomes among individuals diagnosed with COVID-19, hypothesizing differential age structure, underlying health, and work and living arrangements as contributors to inequalities. Using large-scale administrative data from Chicago and adjusting for covariates, we found substantial racial-ethnic and gender identity disparities in both outcomes, and weak evidence of sexual minority disparities in unmet needs. Subsequent decomposition analyses revealed that living in larger households, having a higher share of non-adult cases, and facing higher burdens of chronic illness, obesity, and unemployment each statistically significantly drove racial-ethnic disparities in unmet needs, but these together explained less than 15% of the disparities. Similarly, about 20% of the Black-White gap in hospitalization resulted from disparities in underlying health and unemployment, whereas a higher proportion of non-adult cases or higher unemployment rates respectively proved the only significant pathways to partially explain transgender individuals’ disadvantages in unmet needs (12%) or hospitalization (6%). These findings highlight the importance of considering multiple dimensions of social differences in studying health disparities, the vulnerabilities of transgender and non-adult communities during the pandemic, and the valid yet quite limited roles of previously suggested sociodemographic factors in accounting for COVID-19-related categorical inequalities.
Highlights
-
•
We assessed disparities by unmet needs and hospitalization among COVID-19 cases in Chicago.
-
•
We found stark racial-ethnic and gender identity—but not sexual—minority disparities.
-
•
Several factors statistically contributed to the gaps but with small effect size.
-
•
Underlying health, work and living conditions explained less than 10% of the gaps.
-
•
Minority groups' higher non-adult case load also drove disparities in unmet needs.
Related collections
Most cited references47
- Record: found
- Abstract: not found
- Article: not found
Reconsidering Baron and Kenny: Myths and Truths about Mediation Analysis
- Record: found
- Abstract: found
- Article: found
Longitudinal changes in mental health and the COVID-19 pandemic: evidence from the UK Household Longitudinal Study

- Record: found
- Abstract: found
- Article: found