- Record: found
- Abstract: found
- Article: found
Trends in self-poisoning and psychotropic drug use in people aged 5–19 years: a population-based retrospective cohort study in Australia
Read this article at
Abstract
Objectives
To characterise trends in self-poisoning and psychotropic medicine use in young Australians.
Setting
Calls taken by the New South Wales and Victorian Poisons Information Centres (2006–2016, accounting for 70% of Australian poisoning calls); medicine dispensings in the 10% sample of Australian Pharmaceutical Benefits Scheme data (July 2012 to June 2016).
Main outcome measures
Yearly trends in intentional poisoning exposure calls, substances taken in intentional poisonings, a prevalence of psychotropic use (dispensing of antidepressants, antipsychotics, benzodiazepines and medicines for attention deficit hyperactivity disorder (ADHD)).
Results
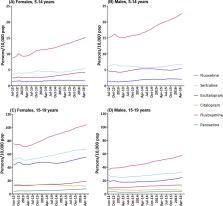
There were 33 501 intentional poisonings in people aged 5–19 years, with an increase of 8.39% per year (95% CI 6.08% to 10.74%, p<0.0001), with a 98% increase overall, 2006–2016. This effect was driven by increased poisonings in those born after 1997, suggesting a birth cohort effect. Females outnumbered males 3:1. Substances most commonly taken in self-poisonings were paracetamol, ibuprofen, fluoxetine, ethanol, quetiapine, paracetamol/opioid combinations, sertraline and escitalopram. Psychotropic dispensing also increased, with selective serotonin reuptake inhibitors (SSRIs) increasing 40% and 35% July 2012 to June 2016 in those aged 5–14 and 15–19, respectively. Fluoxetine was the most dispensed SSRI. Antipsychotics increased by 13% and 10%, while ADHD medication dispensing increased by 16% and 10%, in those aged 5–14 and 15–19, respectively. Conversely, dispensing of benzodiazepines to these age groups decreased by 4% and 5%, respectively.
Conclusions
Our results signal a generation that is increasingly engaging in self-harm and is increasingly prescribed psychotropic medications. These findings indicate growing mental distress in this cohort. Since people who self-harm are at increased risk of suicide later in life, these results may foretell future increases in suicide rates in Australia.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Comparative efficacy and tolerability of antidepressants for major depressive disorder in children and adolescents: a network meta-analysis

- Record: found
- Abstract: found
- Article: found
Hospital Presenting Self-Harm and Risk of Fatal and Non-Fatal Repetition: Systematic Review and Meta-Analysis

- Record: found
- Abstract: found
- Article: found