- Record: found
- Abstract: found
- Article: not found
Face masks against COVID-19: Standards, efficacy, testing and decontamination methods
Read this article at
Abstract
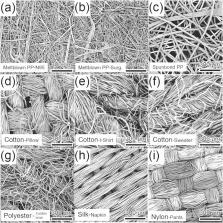
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for the novel coronavirus disease 2019 (COVID-19), has caused a global pandemic on a scale not seen for over a century. Increasing evidence suggests that respiratory droplets and aerosols are likely the most common route of transmission for SARS-CoV-2. Since the virus can be spread by presymptomatic and asymptomatic individuals, universal face masking has been recommended as a straightforward and low-cost strategy to mitigate virus transmission. Numerous governments and public health agencies around the world have advocated for or mandated the wearing of masks in public settings, especially in situations where social distancing is not possible. However, the efficacy of wearing a mask remains controversial. This interdisciplinary review summarizes the current, state-of-the-art understanding of mask usage against COVID-19. It covers three main aspects of mask usage amid the pandemic: quality standards for various face masks and their fundamental filtration mechanisms, empirical methods for quantitatively determining mask integrity and particle filtration efficiency, and decontamination methods that allow for the reuse of traditionally disposable N95 and surgical masks. The focus is given to the fundamental physicochemical and engineering sciences behind each aspect covered in this review, providing novel insights into the current understanding of mask usage to curb COVID-19 spread.
Abstract
Related collections
Most cited references155
- Record: found
- Abstract: found
- Article: not found
Stability of SARS-CoV-2 in different environmental conditions
- Record: found
- Abstract: found
- Article: not found
Airborne transmission of SARS-CoV-2: the world should face the reality
- Record: found
- Abstract: found
- Article: found