- Record: found
- Abstract: found
- Article: found
Decreasing Psychiatric Emergency Visits, but Stable Addiction Emergency Visits, During COVID-19—A Time Series Analysis 10 Months Into the Pandemic
Read this article at
Abstract
Background: The COVID-19 pandemic has been suspected to increase mental health problems, but also to possibly lead to a decreased treatment seeking, for example due to fear of attending hospital. Early findings demonstrate decreased treatment seeking for mental health, which may differ across diagnostic groups. This study aimed to examine treatment uptake at a general psychiatry emergency unit and at an addiction psychiatry emergency unit in Malmö, Sweden, separately. In addition, the study aimed to investigate treatment uptake for different diagnostic groups—during and prior to the COVID-19 pandemic.
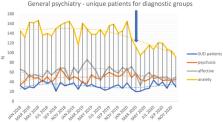
Methods: Monthly data for number of unique patients and number of contacts were extracted for the three-year period of January 2018 through December 2020. Data from each facility were analyzed separately for women, men and patients with psychotic, affective, anxiety and substance use-related disorders. Interrupted time series were used to demonstrate possible effects of COVID-19.
Results: COVID-19 was associated with a marked decrease in treatment contacts, both for women and men, in the general psychiatry emergency unit—driven by a significant decrease in anxiety-related disorders ( p < 0.001) and affective disorders ( p < 0.01)—but not in psychotic or substance use disorders (SUDs). Also, in the addiction psychiatry emergency unit, no significant impact of COVID-19 was seen.
Conclusions: COVID-19 may decrease treatment uptake for acute affective and anxiety-related disorders. Given the hypothesized increase in the population regarding these conditions, societal efforts are needed to facilitate adequate treatment for these patients during the COVID-19 pandemic. Society should also remain vigilant with respect to SUDs during the pandemic.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: found
Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science
- Record: found
- Abstract: found
- Article: found
Collateral damage of COVID‐19 pandemic: Delayed medical care
- Record: found
- Abstract: found
- Article: not found