- Record: found
- Abstract: found
- Article: found
Impact of biomass fuel exposure from traditional stoves on lung functions in adult women of a rural Indian village
Read this article at
Abstract
Introduction:
Exposure to biomass fuel (BMF) from traditional cookstoves inflicts an enormous burden of morbidities in women across the developing world. This study aims to assess the lung function and its association with the indoor air pollutants generated using BMF.
Materials and Methods:
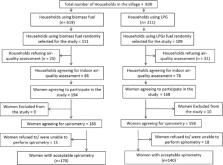
This cross-sectional study including 310 women was conducted in a rural village of India. Households were divided into two groups based on the cooking fuel, the BMF group and the liquefied petroleum gas (LPG) group. Information on respiratory symptoms and socioeconomic status was obtained using a standard questionnaire. Indoor air concentration for PM 10 and PM 2.5 was measured during cooking hours. Pulmonary function tests (PFTs) were conducted for the women inhabitants.
Results:
On comparing the two groups, the concentration of PM 10 (890.26 ± 59.59 vs. 148.66 ± 31.97) μg/m 3 and PM 2.5 (728.90 ± 50.20 vs. 99.76 ± 41.80) μg/m 3 ( P < 0.01) were higher in the group using BMF. The respiratory symptoms such as wheezing, dyspnea, chronic cough, and nocturnal cough, were significantly more common in the group using BMF. A significant difference was seen in the lung function indices between the two groups. A significant negative correlation of respiratory indices with duration of exposure and the particulate matter (PM) values suggested a greater decline on lung function among women exposed to increased concentrations of PM. On comparing participants with normal and abnormal PFT, it was seen that the use of BMF (odds ratio [OR] 8.01; 95% confidence interval [CI] 4.80, 13.36, P < 0.001) and the duration of exposure to BMF (OR 1.16; 95% CI 1.13, 1.20., P < 0.001) increased the odds of having an abnormal PFT.
Related collections
Most cited references27
- Record: found
- Abstract: not found
- Article: not found
The world health report 2002 - reducing risks, promoting healthy life.
- Record: found
- Abstract: found
- Article: not found
