- Record: found
- Abstract: found
- Article: found
Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan
Read this article at
Abstract
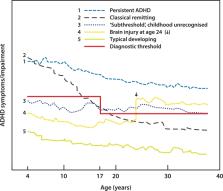
Attention-deficit/hyperactivity disorder (ADHD) is highly heritable and the most common neurodevelopmental disorder in childhood. In recent decades, it has been appreciated that in a substantial number of cases the disorder does not remit in puberty, but persists into adulthood. Both in childhood and adulthood, ADHD is characterised by substantial comorbidity including substance use, depression, anxiety, and accidents. However, course and symptoms of the disorder and the comorbidities may fluctuate and change over time, and even age of onset in childhood has recently been questioned. Available evidence to date is poor and largely inconsistent with regard to the predictors of persistence versus remittance. Likewise, the development of comorbid disorders cannot be foreseen early on, hampering preventive measures. These facts call for a lifespan perspective on ADHD from childhood to old age. In this selective review, we summarise current knowledge of the long-term course of ADHD, with an emphasis on clinical symptom and cognitive trajectories, treatment effects over the lifespan, and the development of comorbidities. Also, we summarise current knowledge and important unresolved issues on biological factors underlying different ADHD trajectories. We conclude that a severe lack of knowledge on lifespan aspects in ADHD still exists for nearly every aspect reviewed. We encourage large-scale research efforts to overcome those knowledge gaps through appropriately granular longitudinal studies.
Related collections
Most cited references199
- Record: found
- Abstract: found
- Article: not found
The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies.
- Record: found
- Abstract: found
- Article: not found
ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis.
- Record: found
- Abstract: found
- Article: found