- Record: found
- Abstract: found
- Article: found
A systematic review of the role of clozapine for severe borderline personality disorder

Read this article at
Abstract
Rationale
Clozapine is a unique medication with a potential role in the treatment of severe borderline personality disorder (BPD).
Objectives
The review examines the effectiveness of clozapine as a medication for management for severe BPD with high risk of suicide, violence or imprisonment, and aims to help guide clinical practice in managing severe BPD.
Methods
A database search of the terms “Clozapine” AND “BPD”; “Antipsychotics” AND “BPD”; “Clozapine” AND “Borderline Personality Disorder”; and “Antipsychotics” AND “Borderline Personality Disorder” were performed in CINAHL, Cochrane Library, Embase, Medline, PsychINFO, PubMed, and Web of Science. Full-text articles of clinical clozapine use for BPD were included for review.
Results
A total of 24 articles consisting of 1 randomised control trial, 10 non-controlled trials, and 13 case reports were identified. Most of the studies reported benefits from clozapine when used for severe BPD. Many of the studies focused on clozapine use in BPD patients at high risk of suicide. Results from these non-controlled and case reports support the use of clozapine in patients with severe BPD at high risk of suicide.
Related collections
Most cited references60
- Record: found
- Abstract: not found
- Article: not found
Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.
- Record: found
- Abstract: found
- Article: found
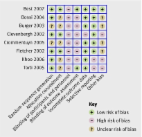
The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials

- Record: found
- Abstract: found
- Article: found