- Record: found
- Abstract: found
- Article: found
Seroprevalence of leptospirosis among blood donors in an endemic area
Read this article at
Abstract
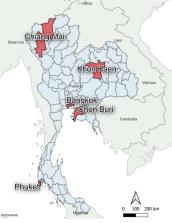
Thailand is known to be endemic for leptospirosis. This bacterium may pose a potential risk to transfusion safety. This study was a cross-sectional study examining the seroprevalence of leptospirosis among Thai blood donors. A total of 1053 serum specimens collected from blood donors residing in 5 regions of Thailand during March to September 2020 were included in this study. All samples were tested for the presence of antibodies to 22 leptospiral serovars using the microscopic agglutination test (MAT) and anti- Leptospira IgG antibodies using commercially available enzyme immunoassay. We found no evidence of recent exposure to Leptospira spp. in sera of healthy Thai blood donors by MAT, including those in higher-risk areas. However, in this same group, we did find small numbers of past exposure (1.7%) to Leptospira spp . by IgG ELISA. According to the findings of this study, there is currently no evidence for implementing new blood banking procedures to identify possible carriers in Thailand, however these should be continually monitored and revised according to the infectious disease burden in each country. It should be noted that there was a difference in the occupation rate between the general population reported in Thailand and blood donors in this study; it may not reflect the actual situation in the country.
Related collections
Most cited references41

- Record: found
- Abstract: found
- Article: found
Global Morbidity and Mortality of Leptospirosis: A Systematic Review
- Record: found
- Abstract: found
- Article: not found