- Record: found
- Abstract: found
- Article: found
Maternal mental illness and child atopy: a UK population-based, primary care cohort study
Read this article at
Abstract
Background
The number of children exposed to maternal mental illness is rapidly increasing and little is known about the effects of maternal mental illness on childhood atopy.
Aim
To investigate the association between maternal mental illness and risk of atopy among offspring.
Design and setting
Retrospective cohort study using a UK primary care database (674 general practices).
Method
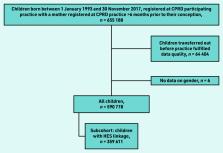
In total, 590 778 children (born 1 January 1993 to 30 November 2017) were followed until their 18th birthday, with 359 611 linked to their hospital records. Time-varying exposure was captured for common (depression and anxiety), serious (psychosis), addiction (alcohol and substance misuse), and other (eating and personality disorder) maternal mental illness from 6 months before pregnancy. Using Cox regression models, incidence rates of atopy were calculated and compared for the exposed and unexposed children in primary (asthma, eczema, allergic rhinitis, and food allergies) and secondary (asthma and food allergies) care, adjusted for maternal (age, atopy history, smoking, and antibiotic use), child (sex, ethnicity, and birth year/season), and area covariates (deprivation and region).
Results
Children exposed to common maternal mental illness were at highest risk of developing asthma (adjusted hazard ratio [aHR] 1.17, 95% confidence interval [CI] = 1.15 to 1.20) and allergic rhinitis (aHR 1.17, 95% CI = 1.13 to 1.21), as well as a hospital admission for asthma (aHR 1.29, 95% CI = 1.20 to 1.38). Children exposed to addiction disorders were 9% less likely to develop eczema (aHR 0.91, 95% CI = 0.85 to 0.97) and 35% less likely to develop food allergies (aHR 0.65, 95% CI = 0.45 to 0.93).
Conclusion
The finding that risk of atopy varies by type of maternal mental illness prompts important aetiological questions. The link between common mental illness and childhood atopy requires GPs and policymakers to act and support vulnerable women to access preventive (for example, smoking cessation) services earlier.
Related collections
Most cited references41

- Record: found
- Abstract: found
- Article: found
The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement

- Record: found
- Abstract: found
- Article: found
Data Resource Profile: Clinical Practice Research Datalink (CPRD)
- Record: found
- Abstract: found
- Article: not found