- Record: found
- Abstract: found
- Article: found
The association between alcohol use, alcohol use disorders and tuberculosis (TB). A systematic review
Read this article at
Abstract
Background
In 2004, tuberculosis (TB) was responsible for 2.5% of global mortality (among men 3.1%; among women 1.8%) and 2.2% of global burden of disease (men 2.7%; women 1.7%). The present work portrays accumulated evidence on the association between alcohol consumption and TB with the aim to clarify the nature of the relationship.
Methods
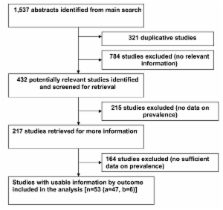
A systematic review of existing scientific data on the association between alcohol consumption and TB, and on studies relevant for clarification of causality was undertaken.
Results
There is a strong association between heavy alcohol use/alcohol use disorders (AUD) and TB. A meta-analysis on the risk of TB for these factors yielded a pooled relative risk of 2.94 (95% CI: 1.89-4.59). Numerous studies show pathogenic impact of alcohol on the immune system causing susceptibility to TB among heavy drinkers. In addition, there are potential social pathways linking AUD and TB. Heavy alcohol use strongly influences both the incidence and the outcome of the disease and was found to be linked to altered pharmacokinetics of medicines used in treatment of TB, social marginalization and drift, higher rate of re-infection, higher rate of treatment defaults and development of drug-resistant forms of TB. Based on the available data, about 10% of the TB cases globally were estimated to be attributable to alcohol.
Related collections
Most cited references118
- Record: found
- Abstract: found
- Article: not found
Alcohol and public health.
- Record: found
- Abstract: found
- Article: not found
Substance abuse and dependence in prisoners: a systematic review.
- Record: found
- Abstract: found
- Article: not found