- Record: found
- Abstract: found
- Article: found
National Antibiotic Consumption for Human Use in Sierra Leone (2017–2019): A Cross-Sectional Study
Read this article at
Abstract
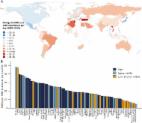
Monitoring antibiotic consumption is crucial to tackling antimicrobial resistance. However, currently there is no system in Sierra Leone for recording and reporting on antibiotic consumption. We therefore conducted a cross-sectional study to assess national antibiotic consumption expressed as defined daily dose (DDD) per 1000 inhabitants per day using all registered and imported antibiotics (categorized under the subgroup J01 under the anatomical and therapeutic classification (ATC) system) as a proxy. Between 2017–2019, total cumulative consumption of antibiotics was 19 DDD per 1000 inhabitants per day. The vast majority consisted of oral antibiotics (98.4%), while parenteral antibiotics made up 1.6%. According to therapeutic/pharmacological subgroups (ATC level 3), beta-lactam/penicillins, quinolones, and other antibacterials (mainly oral metronidazole) comprised 65% of total consumption. According to WHO Access, Watch, and Reserve (AWaRe), 65% of antibiotics consumed were Access, 31% were Watch, and no Reserve antibiotics were reported. The top ten oral antibiotics represented 97% of total oral antibiotics consumed, with metronidazole (35%) and ciprofloxacin (15%) together constituting half of the total. Of parenteral antibiotics consumed, procaine penicillin (32%) and ceftriaxone (19%) together comprised half of the total. Policy recommendations at global and national levels have been made to improve monitoring of antibiotic consumption and antibiotic stewardship.
Related collections
Most cited references37
- Record: found
- Abstract: found
- Article: not found
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies.
- Record: found
- Abstract: found
- Article: not found
Antibiotic resistance-the need for global solutions.
- Record: found
- Abstract: found
- Article: found