- Record: found
- Abstract: found
- Article: found
Glaucoma and Corneal Transplant Procedures
Read this article at
Abstract
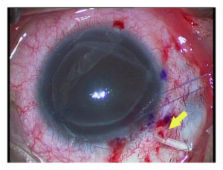
Glaucoma after corneal transplantation is a leading cause of ocular morbidity after penetrating keratoplasty. The incidence reported is highly variable and a number of etiologic factors have been identified. A number of treatment options are available; surgical intervention for IOP control is associated with a high incidence of graft failure. IOP elevation is less frequently seen following deep anterior lamellar keratoplasty. Descemet's striping-automated endothelial keratoplasty is also associated with postprocedure intraocular pressure elevation and secondary glaucoma and presents unique surgical challenges in patients with preexisting glaucoma surgeries. Glaucoma exists in up to three-quarters of patients who undergo keratoprosthesis surgery and the management if often challenging. The aim of this paper is to highlight the incidence, etiology, and management of glaucoma following different corneal transplant procedures. It also focuses on the challenges in the diagnosis of glaucoma and intraocular pressure monitoring in this group of patients.
Related collections
Most cited references87
- Record: found
- Abstract: found
- Article: not found
Descemet's stripping endothelial keratoplasty: safety and outcomes: a report by the American Academy of Ophthalmology.
- Record: found
- Abstract: found
- Article: not found
Corticosteroid-induced glaucoma: a review of the literature.
- Record: found
- Abstract: found
- Article: not found