- Record: found
- Abstract: found
- Article: not found
COVID-19 Infection and Cardiac Arrhythmias
Read this article at
Highlights
-
•
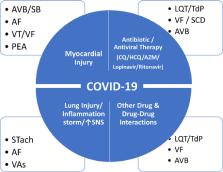
Serious cardiac arrhythmias may be the consequence of direct effects of COVID-19 infection, but also the outcome of the deleterious effects of systemic illness and the adverse proarrhythmic reactions to drugs employed in the treatment of this pandemic
-
•
Drug combinations, especially of QT-prolonging agents, can lead to higher arrhythmogenicity, compared with single drug therapies
-
•
Furthermore, critically ill COVID-19 patients often have comorbidities that can trigger life-threatening ventricular arrhythmias, while acute myocardial injury increases the prevalence of arrhythmias
-
•
ECG and QTc monitoring and taking appropriate measures are of critical importance to prevent, detect and manage cardiac arrhythmias in COVID-19 patients
-
•
Contactless monitoring and telemetry for inpatients, especially those admitted to the ICU, as well as for outpatients needing continued management, has recently been facilitated by implementing digital health monitoring tools
Abstract
As the coronavirus 2019 (COVID-19) pandemic marches unrelentingly, more patients with cardiac arrhythmias are emerging due to the effects of the virus on the respiratory and cardiovascular (CV) systems and the systemic inflammation that it incurs, and also as a result of the proarrhythmic effects of COVID-19 pharmacotherapies and other drug interactions and the associated autonomic imbalance that enhance arrhythmogenicity. The most worrisome of all arrhythmogenic mechanisms is the QT prolonging effect of various anti-COVID pharmacotherapies that can lead to polymorphic ventricular tachycardia in the form of torsade des pointes and sudden cardiac death. It is therefore imperative to monitor the QT interval during treatment; however, conventional approaches to such monitoring increase the transmission risk for the staff and strain the health system. Hence, there is dire need for contactless monitoring and telemetry for inpatients, especially those admitted to the intensive care unit, as well as for outpatients needing continued management. In this context, recent technological advances have ushered in a new era in implementing digital health monitoring tools that circumvent these obstacles. All these issues are herein discussed and a large body of recent relevant data are reviewed.
Related collections
Most cited references78
- Record: found
- Abstract: found
- Article: found
Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China
- Record: found
- Abstract: found
- Article: not found
A Trial of Lopinavir–Ritonavir in Adults Hospitalized with Severe Covid-19

- Record: found
- Abstract: found
- Article: found
