- Record: found
- Abstract: found
- Article: found
Invasive bacterial co-infection in African children with Plasmodium falciparum malaria: a systematic review

Read this article at
Abstract
Background
Severe malaria remains a major cause of pediatric hospital admission across Africa. Invasive bacterial infection (IBI) is a recognized complication of Plasmodium falciparum malaria, resulting in a substantially worse outcome. Whether a biological relationship exists between malaria infection and IBI susceptibility remains unclear. We, therefore, examined the extent, nature and evidence of this association.
Methods
We conducted a systematic search in August 2012 of three major scientific databases, PubMed, Embase and Africa Wide Information, for articles describing bacterial infection among children with P. falciparum malaria using the search string ‘(malaria OR plasmodium) AND (bacteria OR bacterial OR bacteremia OR bacteraemia OR sepsis OR septicaemia OR septicemia).’ Eligiblity criteria also included studies of children hospitalized with malaria or outpatient attendances in sub-Saharan Africa.
Results
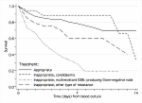
A total of 25 studies across 11 African countries fulfilled our criteria. They comprised twenty cohort analyses, two randomized controlled trials and three prospective epidemiological studies. In the meta-analysis of 7,208 children with severe malaria the mean prevalence of IBI was 6.4% (95% confidence interval (CI) 5.81 to 6.98%). In a further meta-analysis of 20,889 children hospitalised with all-severity malaria and 27,641 children with non-malarial febrile illness the mean prevalence of IBI was 5.58 (95% CI 5.5 to 5.66%) in children with malaria and 7.77% (95% CI 7.72 to 7.83%) in non-malaria illness. Ten studies reported mortality stratified by IBI. Case fatality was higher at 81 of 336, 24.1% (95% CI 18.9 to 29.4) in children with malaria/IBI co-infection compared to 585 of 5,760, 10.2% (95% CI 9.3 to 10.98) with malaria alone. Enteric gram-negative organisms were over-represented in malaria cases, non-typhoidal Salmonellae being the most commonest isolate. There was weak evidence indicating IBI was more common in the severe anemia manifestation of severe malaria.
Conclusions
The accumulated evidence suggests that children with recent or acute malaria are at risk of bacterial infection, which results in an increased risk of mortality. Characterising the exact nature of this association is challenging due to the paucity of appropriate severity-matched controls and the heterogeneous data. Further research to define those at greatest risk is necessary to target antimicrobial treatment.
Related collections
Most cited references47
- Record: found
- Abstract: not found
- Article: not found
Severe falciparum malaria. World Health Organization, Communicable Diseases Cluster.
- Record: found
- Abstract: found
- Article: found
Antimicrobial resistance predicts death in Tanzanian children with bloodstream infections: a prospective cohort study
- Record: found
- Abstract: found
- Article: not found