- Record: found
- Abstract: found
- Article: found
Reasons why OCT Global Circumpapillary Retinal Nerve Fiber Layer Thickness is a Poor Measure of Glaucomatous Progression
Read this article at
Abstract
Purpose
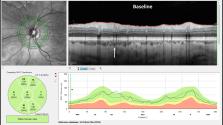
To assess the effects of local defects, segmentation errors, and improper image alignment on the performance of the commonly used optical coherence tomography (OCT) measure of progression, that is the change in global (average) circumpapillary retinal nerve fiber layer (cpRNFL) thickness (ΔG).
Methods
One hundred fifty eyes suspected of, or with, early glaucoma had OCT circle and cube scans obtained using eye tracking on two occasions at least 1 year apart. Statistical progression was defined by fixed values of ΔG (3–8 um) and quantile regression. For a reference standard, four authors identified 30 eyes as “likely progressed,” and 61 eyes that “likely had not progressed” based on OCT reports from both baseline and follow-up tests.
Results
A ΔG criterion of 4 um had the best accuracy: 77%, with 5 false positive (8.2%) and 16 false negative (53%). A post hoc analysis of circular b-scans and OCT probability maps of these eyes indicated that segmentation errors and local progression accounted for most of these mistakes. Segmentation errors, although less common, were also present in true positives and true negatives.
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: found
OCT for glaucoma diagnosis, screening and detection of glaucoma progression
- Record: found
- Abstract: found
- Article: not found
Detecting Structural Progression in Glaucoma with Optical Coherence Tomography.
- Record: found
- Abstract: found
- Article: not found