- Record: found
- Abstract: found
- Article: found
New Highly Active Antiretroviral drugs and generic drugs for the treatment of HIV infection: a budget impact analysis on the Italian National Health Service (Lombardy Region, Northern Italy)
Read this article at
Abstract
Background
In the healthcare sector, it is crucial to identify sustainable strategies in order to allow the introduction and use of innovative technologies. Now, and over the next few years, the expiry of patents for different antiretroviral drugs offers an opportunity to increase the efficiency of resources allocation. The aim of the present study was to assess the impact, on the budget of the Italian National Healthcare Service, of generic antiretroviral drugs and of new antiretroviral drugs entering the market from 2015 to 2019.
Methods
A budget impact model was developed in order to forecast the rate of use of ARTs, based on trends observed within the Lombardy Region (Italy), on clinical experts’ opinion, and the consequent impact on the Italian NHS budget in a five year time horizon. Different scenarios were developed, considering the sole introduction of generic drugs, of new drugs, and their cumulative effects. A multivariate sensitivity analysis was also performed.
Results
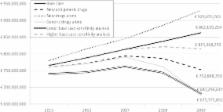
The cumulative use of generic drugs and new drugs would lead to annual savings of 4.6 million € (-0.6 %) in 2015; 16.9 million € (-2.1 %) in 2016; 19.4 million € (-2.4 %) in 2017; 51.1 million € (-6.1 %) in 2018 and -110.3 million € (-12.8 %) in 2019. The impact of new drugs in percentage terms is +2.0 % in 2015, +3.4 % in 2016, +3.9 % in 2017, +5.7 % in 2018 and +7.7 % in 2019. The impact of generic drugs would lead to savings of 4.9 million € in 2015, 18.6 million € in 2016, 22.8 million € in 2017, 76.5 million € in 2018 and 187.4 million € in 2019.
The sensitivity analysis showed annual mean savings for the Italian NHS ranging from 12.6 million €, -1.5 % compared to the base case scenario (decreasing all the rates of transition used in the simulation, and increasing the cost of generic drugs) to 76.0 million €, -9.1 % (increasing all the rates of transition used in the simulation, and decreasing the cost of generic and new drugs).
Related collections
Most cited references11
- Record: found
- Abstract: found
- Article: not found
Delivering affordable cancer care in high-income countries.
- Record: found
- Abstract: not found
- Article: not found
HIV drug development: the next 25 years.
- Record: found
- Abstract: found
- Article: not found